Published 2021-07-12
Keywords
- Pediatric,
- Urinary Tract Infections,
- Clinical Approach
How to Cite
Copyright (c) 2021 McGill Journal of Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Abstract
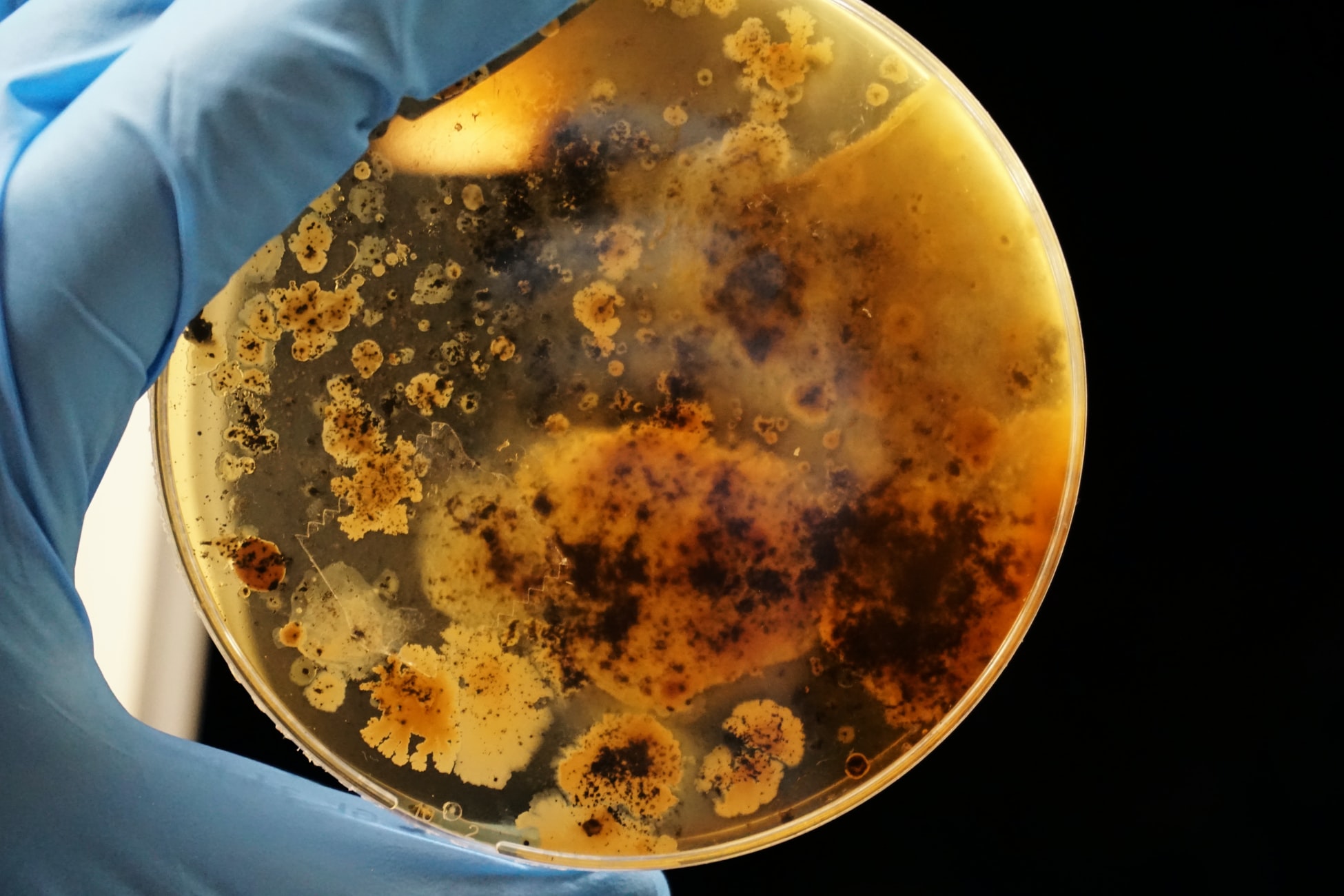
Urinary tract infections (UTIs) are prevalent in the children. Presentation of UTI vary in children of different ages. In infants, who cannot localize symptoms, UTI can present with a fever whereas in older children a UTI can present with urinary symptoms (dysuria, urinary frequency, incontinence). It is important to establish a clear diagnosis in order to treat and resolve the infection with antibiotics therapy to prevent bacteremia, pyelonephritis, and long-tern renal disease. Urine is collected through a mid-stream urine sample, in toilet trained children, via urethral catheterization, suprapubic aspiration and pediatric urine collection bags. Urine analysis and culture are the first-line investigations in children with suspected UTI. Goals of treatment include elimination of infection, relief of acute symptoms, and prevention of recurrent and long-term complications. The Canadian Pediatric Society recommends initial treatment with oral antibiotics for nontoxic children with febrile UTIs. Imaging, such as a renal/bladder ultrasound, may be used.
Downloads
References
- Schlager TA. Urinary tract infections in children younger than 5 years of age: epidemiology, diagnosis, treatment, outcomes and prevention. Paediatr Drugs. 2001;3(3):219-27.
- Simões e Silva AC, Oliveira EA. Update on the approach of urinary tract infection in childhood. J Pediatr (Rio J). 2015;91(6 Suppl 1):S2-10.
- Balighian E, Burke M. Urinary Tract Infections in Children. Pediatr Rev. 2018;39(1):3-12.
- Robinson JL, Finlay JC, Lang ME, Bortolussi R. Urinary tract infections in infants and children: Diagnosis and management. Paediatr Child Health. 2014;19(6):315-25.
- Shaikh N, Morone NE, Bost JE, Farrell MH. Prevalence of urinary tract infection in childhood: a meta-analysis. Pediatr Infect Dis J. 2008;27(4):302-8.
- Leung AKC, Wong AHC, Leung AAM, Hon KL. Urinary Tract Infection in Children. Recent Pat Inflamm Allergy Drug Discov. 2019;13(1):2-18.
- Morello W, La Scola C, Alberici I, Montini G. Acute pyelonephritis in children. Pediatr Nephrol. 2016;31(8):1253-65.
- Shaikh N, Morone NE, Lopez J, Chianese J, Sangvai S, D'Amico F, et al. Does this child have a urinary tract infection? Jama. 2007;298(24):2895-904.
- May OW. Urine Collection Methods in Children: Which is the Best? Nurs Clin North Am. 2018;53(2):137-43.
- Al-Orifi F, McGillivray D, Tange S, Kramer MS. Urine culture from bag specimens in young children: are the risks too high? J Pediatr. 2000;137(2):221-6.
- Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128(3):595-610.
- Hoberman A, Charron M, Hickey RW, Baskin M, Kearney DH, Wald ER. Imaging studies after a first febrile urinary tract infection in young children. N Engl J Med. 2003;348(3):195-202.
- Zhang X, Xu H, Zhou L, Cao Q, Shen Q, Sun L, et al. Accuracy of early DMSA scan for VUR in young children with febrile UTI. Pediatrics. 2014;133(1):e30-8.
- Leroy S, Fernandez-Lopez A, Nikfar R, Romanello C, Bouissou F, Gervaix A, et al. Association of procalcitonin with acute pyelonephritis and renal scars in pediatric UTI. Pediatrics. 2013;131(5):870-9.




