Original Research
Access to Immunoglobulin Treatment for CIDP Patients During the COVID-19 Pandemic
Vincent Brissette1,
Laurence Poirier2,
Rami Massie3,
Colin Chalk3,
Fraser Moore4,
Published online: August 25th, 2023
1Faculty of Medicine and Health Sciences, McGill University, Montreal, Quebec Canada
2University of Ottawa, Department of Neurology, Faculty of Medicine, Ottawa, Ontario, Canada
3Department of Neurology and Neurosurgery, Montreal Neurological Hospital, McGill University, Montreal, Quebec, Canada
4Department of Neurology and Neurosurgery, Jewish General Hospital, McGill University, Montreal, Quebec, Canada
Corresponding Author: Vincent Brissette, email vincent.brissette@mail.mcgill.ca
DOI: 10.26443/mjm.v21i1.964
Abstract
Background: Immunoglobulin supplies are limited; their access for patients diagnosed with chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) may have been difficult during the COVID-19 pandemic.
Methods: A retrospective cross-sectional study was conducted with CIDP patients (n=16, 68.8% female, mean age 60.4±11.3) recruited from three Montreal tertiary care institutions. Inclusion criteria were patients over 18 years old who were receiving immunoglobulin treatment as of March 1st, 2020. Patients were asked to complete a questionnaire inquiring about changes in their immunoglobulin treatment during the pandemic and about their quality of life. Their charts were reviewed by an independent investigator. We used weighted chi-squared statistical tests and Cramer’s V correlation ratios to measure associations with treatment change.
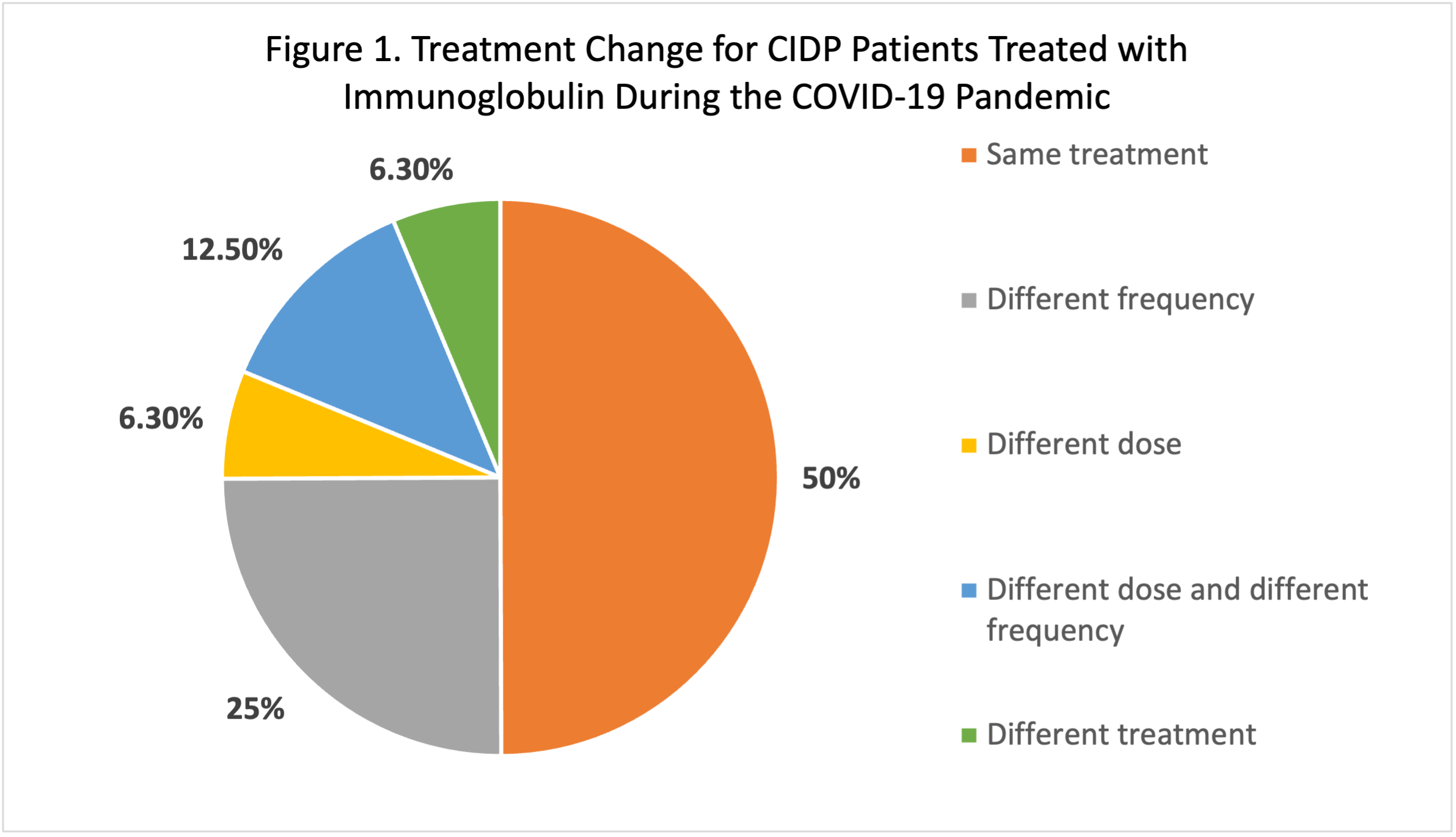
Results: Eighteen months after the pandemic started, 50% of patients were receiving the same treatment, 25% were receiving immunoglobulin treatment at a different frequency, 6.3% were receiving a different dose, 12.5% were receiving a different dose and frequency, and 6.3% were receiving a different treatment. Reasons associated with treatment change were worsening of neurological condition (18.8%; Cramer’s V=0.480; p-value=0.055), improvement of neurological condition (25%; Cramer’s V=0.577; p-value=0.021) and reduced availability of treatment (6.3%; Cramer’s V=0.258; p-value=0.302). There were no significant correlations between lower quality of life (p-value=0.323) or lower Rasch-built Overall Disability Scale score (p-value=0.574) and treatment change.
Conclusion: Difficulty accessing immunoglobulin treatment was infrequent and not significantly associated with treatment change for CIDP patients during the COVID-19 pandemic. A larger multicentre study across multiple sites might identify other treatment access problems resulting from the pandemic.
Tags: COVID-19, CIDP, neuromuscular diseases
Introduction
Access to care for some patients with neuromuscular conditions has become a challenge during the COVID-19 pandemic [1]. Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) is an immune-mediated neuropathy defined by clinical progression for more than 2 months, and electrodiagnostic evidence of peripheral nerve demyelination [2]. Immunoglobulin treatment is considered a first-line treatment for patients with CIDP [3].
Various factors may have limited access to immunoglobulin during the pandemic including social distancing, cancellation of blood drives [4, 5], reduced donor availability, reduced availability of personnel trained to collect and manufacture blood products [6, 7], and reallocation of healthcare resources [8]. Reduced blood product inventory has been reported both in Canada [9] and in the United States [4] during the pandemic. Patients themselves may have been reluctant to attend healthcare facilities due to fear of contracting COVID-19. Patients with CIDP have reported similar concerns [10], and some patients have tried to discontinue or change their treatment course for safety reasons [11]. Finally, a proposition to promote patient-administered subcutaneous over intravenous immunoglobulin treatment was recommended during the pandemic to help reduce the movement of people and the potential spread of the virus [11].
The goal of this study was to determine whether the pandemic was associated with changes in immunoglobulin treatment access for CIDP patients.
Methods
Study design
After institutional ethics board approval, we conducted an observational cross-sectional study of CIDP patients treated with immunoglobulin. We followed the STROBE guideline in reporting our findings to help in bias identification [12].
Patient identification and inclusion criteria
Sixteen patients were recruited with convenience sampling from three academic tertiary care institutions in Montreal, QC, Canada: the Jewish General Hospital, the Montreal Neurological Institute, and the Montreal General Hospital. Patients were identified from lists maintained by the treating neurologists. All patients meeting inclusion criteria were invited to participate by their treating physicians.
Inclusion criteria were: age ≥ 18 years old; diagnosis of CIDP; and active treatment with immunoglobulin (subcutaneous or intravenous) as of March 1st, 2020. Patients were invited to participate by their treating physician or by phone by a member of the research team after physician referral.
Data collection
Eligible patients were invited to complete an in-person or online questionnaire inquiring about treatment changes 18 months after the start of the pandemic (September 1st, 2021). The questionnaire collected basic information about patient characteristics and demographics, treatment change compared to the beginning of the pandemic (March 1st, 2020), and reasons for treatment change if applicable. We used the linearly weighted R-ODS (Rasch-built Overall Disability) scale to collect information on activity and social limitations during the COVID-19 pandemic. The scale asks about a wide range of activities and has been used with patients with different levels of functional limitations due to Guillain-Barré Syndrome (GBS), CIDP, and Monoclonal Gammopathy of Underdetermined Significance (MGUSP) [13]. We also collected information on the patient’s reported quality of life (greatly impaired (1), slightly impaired (2), average (3), good (4), and excellent (5)) and on the patient’s reported level of physical activity (low (1), moderate (2), and high(3)) as both are direct or indirect predictors of overall function [14]. Patient charts were reviewed by an independent investigator not directly involved in patient care, who then completed a physician questionnaire.
Data analysis
Our primary objective was to determine whether changes in treatment occurred during the COVID-19 pandemic and what the reasons for these changes were. Our secondary objectives were to identify if overall disability (R-ODS score), reported quality of life, and level of physical activity were associated with treatment change and with reasons for treatment change. If an association was established, our third objective was to evaluate the strength of such association with correlation coefficients.
To analyze associations between the dichotomous dependent variable “treatment change” and the independent categorical variable “reasons for treatment change”, we used the chi-squared statistical test (𝟀2). We used the Cramer’s V correlation ratio to evaluate the strength of established associations [15]. We used the chi-squared statistical test and the Cramer’s V correlation ratio to evaluate associations between other categorical variables (reported quality of life and level of physical activity) and our main outcome “treatment change”, and we used the point-biserial correlation coefficient (rPB) to evaluate its association with the continuous variable overall disability (R-ODS score) [16]. We defined statistical significance as a p-value <0.05 and conducted our analyses with IBM SPSS Statistics v.28.0 (IBM Corp., Armonk, New York, United States) [17].
Results
Twenty-seven patients were identified from the treating neurologists’ lists. Seven patients were excluded by the independent investigator due to failure to meet inclusion criteria after further chart review (e.g., patients were started on intravenous immunoglobulin (IVIG) after March 1st, 2020), two patients refused to participate or were unable to participate, and two patients could not be reached. Sixteen patients were included for analysis.
Characteristics of our study population were: 68.8% female, age 60.38 ± 11.31, mean quality of life 2.75 ± 1.39, mean level of physical activity 1.5 ± 0.63, mean R-ODS score 33.75 ± 9.11, mean motor conduction velocity of the right ulnar nerve at original diagnosis 41.15 ± 16.79 m/s, and mean CSF protein value at original diagnosis 1.21 ± 0.56 g/L. Comorbidities included end-stage renal disease (1 patient), hypothyroidism (3 patients), vitamin B12 deficiency (2 patients), cancer treated with chemotherapy (2 patients), and diabetes (2 patients) (Table 1).
| Table 1: Characteristics of our Study Population | Mean | SD | |
|
Gender (%) Male Female Age (years) Quality of life Level of physical activity R-ODS Score Mean CV* of right ulnar nerve at diagnosis (m/s) Greatest reduction in CV at diagnosis (m/s) Mean CSF** protein value (g/L) Comorbidities (number of patients) ESRD** Hypothyroidism Vitamin B12 deficiency Cancer treated with chemotherapy Diabetes |
31.25 68.75 60.38 2.75 1.50 33.75 41.15 21.85 1.21
1 3 2 2 2 |
- - ±11.31 ±1.39 ±0.63 ±9.11 ±16.79 ±10.56 ±0.56
- - - - - |
|
|
*CV: conduction velocity **CSF: cerebrospinal fluid ***ESRD: End-stage renal disease |
|||
Eighteen months after the pandemic started (using a start date of March 1st, 2020, for our region), 8 patients (50%) were receiving the same treatment, 4 patients (25%) were receiving immunoglobulin treatment at a different frequency, 1 patient (6.3%) was receiving a different dose of immunoglobulin treatment, 2 patients (12.5%) were receiving a different dose and a different frequency, and 1 patient (6.3%) was receiving a treatment other than immunoglobulin therapy (Figure 1). Reasons associated with treatment change were worsening of neurological condition (18.8%; Cramer’s V=0.480; p-value=0.055), improvement of neurological condition (25%; Cramer’s V=0.577; p-value=0.021) and reduced availability of treatment (6.3%; Cramer’s V=0.258; p-value=0.302) (Table 2).
| Table 2: Reasons Associated with Treatment Change | Reason | % of our population | p-value | Cramer’s V |
|
Worsening of neurological condition Improvement of neurological condition Reduced availability of treatment |
18.8 25 6.3 |
0.055 0.021 0.302 |
0.480 0.577 0.258 |
We analyzed associations between R-ODS score, quality of life, and level of physical activity with treatment change and reasons for treatment change. No statistically significant associations were found. (Table 3)
| Table 3: Associations Between Quality of Life, Physical Activity, and R-ODS Score and Treatment Change and Reasons for Treatment Change | Quality of life | Physical activity | R-ODS score | p-value | Cramer’s V | p-value | Cramer’s V | p-value | rPB* |
| Treatment change | 0.323 | 0.54 | 0.411 | 0.333 | 0.835 | 0.057 |
| No treatment change | 0.323 | 0.54 | 0.411 | 0.333 | 0.835 | -0.057 |
| Worsening of neurological condition | 0.123 | 0.673 | 0.853 | 0.141 | 0.333 | -0.259 |
| Improvement of neurological condition | 0.695 | 0.373 | 0.196 | 0.451 | 0.429 | 0.213 |
| Reduced availability of immunoglobulin | 0.525 | 0.447 | 0.660 | 0.228 | 0.570 | 0.154 |
| Change to a different treatment | 0.777 | 0.333 | 0.660 | 0.228 | 0.235 | -0.315 |
|
*rPB = point-biserial correlation coefficient |
||||||
Discussion
We found no association between changes in immunoglobulin treatment for CIDP patients during the COVID-19 pandemic and reduced availability or difficulty accessing immunoglobulin. We also found no significant association between R-ODS score, level of physical activity, or quality of life with reasons for treatment change.
Although reduced inventory of blood products including immunoglobulin was reported during the pandemic, most of the decline in blood product collection in Canada was between February 2020 and May 2020, with a robust recovery by December 2020. Pre-pandemic, 70,000 donors were able to attend donor centres compared to 54,738 donors in May 2020, and 72,853 by December 2020 [9]. By the fourth quarter of 2020, whole blood collections were almost back to pre-pandemic levels: 190,000 collections compared to the pre-pandemic baseline of 200,000 collections [18]. Therefore, rapid adaptations of blood centres to public health measures, ongoing commitment to blood donation during the pandemic, and changes in donor selection criteria (such as reducing the hemoglobin threshold acceptable for donation) could explain why our patients did not experience reduced immunoglobulin treatment availability [9].
One patient did report reduced availability of IVIG as a reason for change in treatment. After chart review, the actual reason for treatment change was improvement of neurological condition. Fears about suspected impacts of the pandemic may have contributed to our patient’s misconception; news reports of decreased blood product reserves were common during the first few months of the pandemic [9]. A study with 29 adult CIDP patients reported pronounced psychological distress during the COVID-19 outbreak, with 27% of patients reporting concerns about drug availability and 20% reporting concerns about hospital accessibility [10]. Another study reported increased anxiety and feelings of loneliness for patients with neuromuscular diseases [19].
Patients with other chronic neurological conditions also faced impaired access to their care during the pandemic and resulting consequences: patients with migraines have been facing difficulty in accessing care and increased headache frequency [20]; patients with epilepsy with high seizure frequency and difficulty obtaining proper medical care reported depressive symptoms [21]; and patients with dementia experienced worsening cognitive, behavioral and psychological symptoms with disruption of their care [22]. Therefore, while immunoglobulin accessibility has not been directly affected, it is still possible that patients with CIDP faced difficulties and alterations in their normal care access in association with the pandemic. Examples include the development of concomitant COVID-19 infection, global safety measures affecting access to physical rehabilitation, mandatory social isolation [1], and the increasing use of telemedicine [23, 24].
Although our study showed no significant association between R-ODS score, level of physical activity, or quality of life with treatment change, other studies have shown that the COVID-19 pandemic did impact quality of life for CIDP patients and others. The pandemic was negatively associated with CIDP patients’ daily activities and associated with lower sleep quality [10] which is a predictor of quality of life [25]. An international survey with thirty-five research organizations across the world showed that home confinement had a negative effect on physical activity level for people in general and led to increased daily sitting time [26]. Physical activity is associated with better quality of life, lower sensory impairment, and reduced disability measured by R-ODS score for CIDP patients [14]; it is possible that CIDP patients had reduced activity levels and therefore a lower overall quality of life during the pandemic.
Our study features two main strengths: the risk of selection bias was reduced by referring all patients expected to meet inclusion criteria prior to looking for treatment change in their charts, and reporting bias was reduced by reporting all findings, including not statistically significant findings. Our study’s main limitation is the small sample size that may have led to an underestimation of the true association between treatment changes and reduced availability of treatment [27]. In fact, due to a significant sampling bias, our small group of patients may not be fully representative of treatment issues experienced by all CIDP patients during the pandemic. Similarly, while our study included patients from three academic tertiary care institutions, all institutions were in the same city (Montreal, QC, Canada), undermining potential treatment access difficulties experienced by patients in more remote areas or different cities. Our study focused solely on patients treated with immunoglobulin and how their immunoglobulin treatment was affected; we did not try to detect other associations between the pandemic and impaired access to care for CIDP patients. Finally, patients newly diagnosed during the pandemic were excluded because achieving successful treatment may take some time for new CIDP patients and require multiple changes that would have influenced our main objective, that is to evaluate how the pandemic affected patients already under treatment. Hence, it is possible that CIDP patients encountered greater barriers to treatment.
In conclusion, difficulty accessing immunoglobulin treatment was infrequent in our population and not significantly associated with treatment change for CIDP patients during the COVID-19 pandemic. We found no association between quality of life, physical activity, or R-ODS score and reasons for treatment change. Our study highlights important points to learn from the COVID-19 pandemic: a reduced inventory of blood products including immunoglobulin was reported during the pandemic, patients reported concerns about drug availability during the pandemic, patients with neurological conditions faced impaired access to their care during the pandemic, and studies have shown that the COVID-19 pandemic impacted the quality of life of CIDP patients. A larger multicentre study across multiple sites could identify treatment access difficulties not limited to immunoglobulin, and further evaluate associations between patients’ quality of life and treatment access difficulties. This could help justify providing them with greater resources, if needed.
References
- Bertran Recasens, B. and M.A. Rubio, Neuromuscular Diseases Care in the Era of COVID-19. Front Neurol, 2020. 11: p. 588929.
- Kuwabara, S. and S. Misawa, Chronic Inflammatory Demyelinating Polyneuropathy. Adv Exp Med Biol, 2019. 1190: p. 333-343.
- European Federation of Neurological Societies/Peripheral Nerve Society Guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society--First Revision. J Peripher Nerv Syst, 2010. 15(1): p. 1-9.
- Cross, A.R. American Red Cross Faces Severe Blood Shortage As Coronavirus Outbreak Threatens Availability of Nation’s Supply. 2020 [cited 2021 October 20th]; Available from: https://www.redcross.org/about-us/news-and-events/press-release/2020/american-red-cross-faces-severe-blood-shortage-as-coronavirus-outbreak-threatens-availability-of-nations-supply.html.
- Reporter, A. Blood Supply Hits Emergency Level due to Coronavirus Concerns. 2020 [cited 2021 October 20th ]; Available from: https://www.auburn-reporter.com/news/blood-supply-hits-emergency-level-due-to-coronavirus-concerns/.
- Yazer, M.H., et al., Vox Sanguinis International Forum on transfusion services' response to COVID-19: Summary. Vox Sang, 2020. 115(6): p. 536-542.
- Stanworth, S.J., et al., Effects of the COVID-19 pandemic on supply and use of blood for transfusion. Lancet Haematol, 2020. 7(10): p. e756-e764.
- Blackhouse, G., et al., Cost-utility of Intravenous Immunoglobulin (IVIG) compared with corticosteroids for the treatment of Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) in Canada. Cost Eff Resour Alloc, 2010. 8: p. 14.
- Khandelwal, A., Impact of COVID-19 on blood donation in Canada. 2021: Internet.
- Stojanov, A., et al., The influence of the COVID-19 pandemic on patients with chronic inflammatory demyelinating polyradiculoneuropathy. Clin Neurol Neurosurg, 2021. 205: p. 106654.
- Romozzi, M., et al., Reassessing IVIg therapy in chronic inflammatory demyelinating polyradiculoneuropathy during COVID-19: a chance to verify the need for chronic maintenance therapy. Neurol Sci, 2021. 42(3): p. 787-789.
- von Elm, E., et al., The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol, 2008. 61(4): p. 344-9.
- van Nes, S.I., et al., Rasch-built Overall Disability Scale (R-ODS) for immune-mediated peripheral neuropathies. Neurology, 2011. 76(4): p. 337-345.
- Doneddu, P.E., et al., Impact of environmental factors and physical activity on disability and quality of life in CIDP. J Neurol, 2020. 267(9): p. 2683-2691.
- McHugh, M.L., The chi-square test of independence. Biochem Med (Zagreb), 2013. 23(2): p. 143-9.
- The SAGE Encyclopedia of Communication Research Methods. 2017.
- Corp., I., IBM SPSS Statistics for Mac. 2021, IBM Corp.: Armonk, NY.
- Sher, G. Open Board Metting. 2020 [cited 2021 October 30th ]; Available from: https://www.blood.ca/sites/default/files/CEO_Mid_Year_Review_Q1-Q2_2020-2021_-_OBM_Presentation.pdf?_gl=1*1hff888*_ga*NTY2ODYzNzQzLjE2MzU2MjEzNzQ.*_ga_YHMRKTXXVD*MTYzNTYyMTM3NC4xLjEuMTYzNTYyMTU3Ni4w&_ga=2.209525275.807575966.1635621374-566863743.1635621374.
- Consonni, M., et al., Amyotrophic lateral sclerosis patients' and caregivers' distress and loneliness during COVID-19 lockdown. J Neurol, 2021. 268(2): p. 420-423.
- Chowdhury, D. and D. Datta, Managing Migraine in the Times of COVID-19 Pandemic. Ann Indian Acad Neurol, 2020. 23(Suppl 1): p. S33-s39.
- Dos Santos Lunardi, M., et al., Patients with epilepsy during the COVID-19 pandemic: Depressive symptoms and their association with healthcare access. Epilepsy Behav, 2021. 122: p. 108178.
- Toniolo, S., et al., Dementia and COVID-19, a Bidirectional Liaison: Risk Factors, Biomarkers, and Optimal Health Care. J Alzheimers Dis, 2021. 82(3): p. 883-898.
- Hincapié, M.A., et al., Implementation and Usefulness of Telemedicine During the COVID-19 Pandemic: A Scoping Review. J Prim Care Community Health, 2020. 11: p. 2150132720980612.
- Ganapathy, K., Telemedicine and Neurological Practice in the COVID-19 Era. Neurol India, 2020. 68(3): p. 555-559.
- Medic, G., M. Wille, and M.E. Hemels, Short- and long-term health consequences of sleep disruption. Nat Sci Sleep, 2017. 9: p. 151-161.
- Ammar, A., et al., Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients, 2020. 12(6).
- Hackshaw, A., Small studies: strengths and limitations. Eur Respir J, 2008. 32(5): p. 1141-3.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.