Approach to
Headaches
Benjamin Rehany1
Zachary Rehany1
Published online: October 23, 2022
1Faculty of Medicine, McGill University, Montreal, Quebec, Canada
Corresponding Author: Benjamin Rehany, email: benjamin.rehany@mail.mcgill.ca
DOI: 10.26443/mjm.v21i1.958
Abstract
Headaches are one of the most common reasons for visiting a family physician. The estimated lifetime prevalence of a headache is about 66%. (1) They pose a significant burden on the patient’s quality of life, and in fact contribute to about 20% of work absences. (2) Fortunately, most cases are benign. The following article presents an approach to headaches with a focus on migraines. The article aims to differentiate between benign and worrisome causes of headaches and describe the management.
Tags: Headaches, Migraines, Imaging, Family medicine
Question
J is a 27-year-old female university student who works part-time as a waitress. She presents to a family physician office with an 11-month history of intermittent severe headaches. Her past medical history is unremarkable. She has no allergies, and occasionally takes Ibuprofen to which she claims does not help anymore. Her father is diabetic, and her mother is known for high blood pressure.
She began to have headaches at the start of exams last semester. She experiences about 2-3 every month and they each last about 7 hours. Sometimes she stays home from school as because the headaches are so severe. During a headache episode she feels a unilateral throbbing pain around her head, she also feels nauseous and has even vomited on occasion. During the attack she gets very irritable to any loud sound. Fortunately, lying down and closing her eyes helps ease the pain.
On physical exam her BP is 130/86, heart rate 65/min, respiratory rate 15/min. Oral temperature is 37 degrees. No papilledema was identified. No pain was reproduced upon sinus palpation.
The patient denies recent trauma, fever, neck stiffness, night sweats, fatigue, or weight loss. The patient denies any syncope, vertigo, light-headedness, tremor, weakness, paresthesia or speech difficulty. Patient is alert, attentive and oriented. Neurology exam including cranial nerves, motor strength, reflexes, sensation and coordination were within normal limits .
J’s grandfather recently died from cancer and this is causing her to worry that her headaches may be indicative of a harmful underlying condition.
As the family physician, what would be the next best course of action?
- Order an MRI stat to rule out malignancy
- Prescribe a high dose NSAID
- Referral to neurology to evaluate for brain damage
- Reassure the patient and discuss other possible medications
Answer
D. The case is of a young student who is juggling multiple potential stressors. She reports no head trauma, lack of coordination, or numbness and is otherwise in good health. Her headache presented several months ago and has maintained in frequency. The case is a typical presentation of a migraine. While headaches are commonly benign, it is important to complete a thorough history and physical exam to exclude any serious secondary causes. Once the diagnosis with migraines is made, the patient will explore the avenues of treatment and the physician should reassure her that the condition is not life-threatening.
Initial approach
Definition of primary and secondary headaches:
Headaches are divided into two classes, primary and secondary. Primary headaches describe disorders in which the cephalalgia is not due to an underlying lesion. Secondary headaches describe disorders in which the pain is from another underlying cause. Despite 66% of the population experiencing primary headaches at one point in their lives, the etiology is poorly understood. (3) The most widely accepted theory describing primary headaches is that there is sensitization of nociceptive neurons. The long-lasting activation and sensitization of these neurons triggers a headache attack. This can be further explained as a form of disinhibitory sensitization with dysfunction of descending modulatory pathways; a similar mechanism to what occurs in allodynia. The peripheral sensitization of trigeminal nociceptive afferents innervating the dural meninges was seen to be playing the leading role. (3) Specifically, the local release of inflammatory markers were responsible for activating the trigeminal nociceptors. (4)
Important causes of secondary headaches:
While primary headaches constitute 98% of all headaches, it is important to recognize secondary headaches as they can potentially be life threatening. (5) Secondary headaches are those that arise from an underlying structural lesion to the brain and/or the surrounding structures. Etiologies include vascular, infectious, neoplastic, or traumatic causes. Vascular causes include hemorrhages such as subdural hemorrhage, incracerebral hemorrhage and subarachnoid hemorrhage which presents as a sudden severe onset headache is termed a “thunderclap headache.” (6) Subdural hemorrhage and intracerebral hemorrhage are included too. Vascular disorders also include arteriovenous malformations, cerebral venous sinus thrombosis (CVST), collagen vascular disease, carotid artery dissection, arteritis, and others. Infectious causes typically include meningitis and sinus infections. Mass lesions can present with systemic symptoms, seizures and headaches. Trauma to the neck and head can cause direct/indirect structural lesions – namely contusions, skull fracture and edema which can lead to headaches as well. The clinical presentation of secondary headaches will be discussed in further detail.
Red flags for headaches:
While performing the history it is important to keep in mind the most common and most worrisome causes of headaches. The most common being benign such as a tension-type headache while the most worrisome being a subarachnoid hemorrhage or a hypertensive emergency. Signs such as systemic symptoms, neurological symptoms, sudden onset, onset at older age, and change in pattern are red flags that require prompt evaluation for a serious cause. A concise summary of the red flags is shown in Table 1.
| Table 1: Red flags for headaches |
| Systemic symptoms: Fever, night sweats, weight loss |
| Neurological symptoms |
| Sudden severe onset: Need to r/o Thunderclap headache |
| Onset age over 50 |
| Change in Pattern |
| Progressive worsening |
| Other: precipitated by Valsalva, postural aggravation, papilledema |
When a patient presents with pain, such as a headache, it is often instinctual to order imaging tests. Meanwhile, in the case where there are no red flags, imaging is rarely helpful.(7) Utilizing clinical skills can help avoid the risks and the high cost associated with imaging. Having an established clinical approach does not only alleviate the burden on the imaging department but also helps avoid unnecessary tests on the patients.
History and Physical exam:
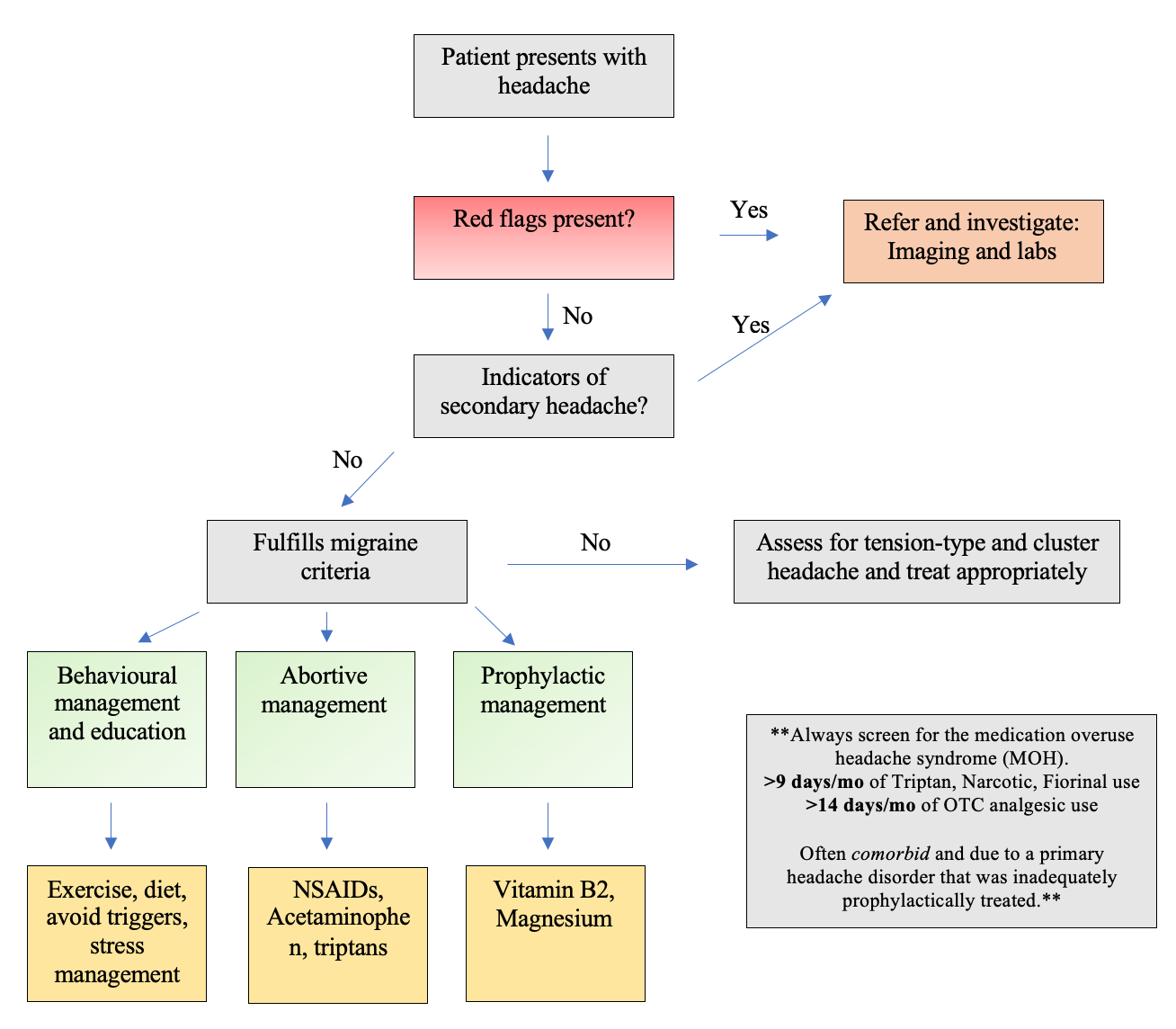
Most headache diagnoses can be made entirely from the patient history and physical exam. A Flowchart summarizing the approach to headaches is found on Flowchart 1. The history should focus on the location, quality, severity, provoking and alleviating factors and length of the headache. Associated symptoms that occur with the headache should be asked as well such as nausea, vomiting or photophobia. The physical exam should focus on the head and neck along with a full neurological exam. The head is examined for any skin changes, bruising and deformities. The scalp should be examined for tenderness and swelling which can be signs of trauma. The conjunctiva and fundi are each examined. The head and neck are palpated for any lesions or lymphadenopathy.
Neurological exam should include a cursory overview of the mental status and language. Cranial nerve exam should include a minimum screening of visual fields, fundoscopy, pupillary light reflexes and visual acuity. Extraocular motility and presence of pathological nystagmus should also be commented on. Lower cranial nerves are to be examined for facial asymmetries, facial sensory loss or hearing impairment (i.e, with finger rub, Weber and Rinne testing). The remainder of the neurological exam should be aimed at identifying if any (presence of) motor asymmetries, limb weakness, changes in tone, or objective anatomically based regions of sensory loss. Abnormal or asymmetrical deep tendon reflexes can help distinguish UMN from LMN, which may facilitate localization to the PNS or CNS. Gait and coordination should be commented on, and is expected to be normal.
Other signs to look out for are especially important to help rule out secondary or worrisome causes of headaches. Some of the common infectious, vascular, neoplastic, and drug-induced aetiologies will be described, divided into broad categories.
Infectious: Headache with fever, nuchal rigidity, photophobia and sometimes mental status change can indicate a headache secondary to meningitis. (8) Meningitis can also be associated with headache and change in personality or mental status. Sinusitis can also lead to headaches, which is why it may be useful to palpate the sinuses on physical exam to evaluate for any reproducible pain.
Vascular: The temporal artery and temporomandibular joints are palpated to evaluate for temporal artery arteritis; a recognizable cause of blindness. Sudden onset with maximal intensity within minutes can indicate a sub-arachnoid hemorrhage. An acute headache with a gradual worsening can point more towards a subdural headache. New onset headache in pregnancy or post-partum can point to cranial venous sinus thrombosis, carotid artery dissection or pituitary apoplexy. (9)
Neoplastic: Papilledema on a fundoscopy exam can indicate signs of increased cranial pressure resulting from hemorrhage or a tumor such as glioblastoma. (10) In severe cases masses can also cause herniation leading to focal neurological signs. Systemic symptoms such as night sweats, fatigue, and weight loss can also be present. Lastly, age is generally an important factor when suspecting a malignancy.
Drug/poisoning: Medication overuse with NSAIDs or acetaminophens has been shown to cause rebound headaches. (11) Carbon monoxide poisoning classically presents with a sudden onset severe headache. (12)
Investigations to exclude secondary causes of headaches:
Laboratory investigations are not diagnostic in the context of primary headaches but help in the suspicion of secondary headaches. Blood investigations: A complete blood count, thyroid function, and erythrocyte sedimentation rate (ESR) should be performed when relevant. A basic metabolic panel including glucose, electrolytes, and kidney function can be ordered. Thyroid function tests are performed as there are increasing studies linking hypothyroidism to headaches. (13) ESR is a marker of inflammation and can increase suspicion of giant cell arteritis, classically in individuals over 50 with new onset headaches. Lastly, in a clinical context of arthritis and headaches antinuclear antibody and rheumatoid factor can be performed. Lumbar tap (LP): an LP would be performed if there is a high clinical suspicion of an infection or subarachnoid hemorrhage. An increasing red cell count would indicate a hemorrhage while a high white cell count points towards infection. Imaging: as with any investigation, imaging should only be ordered in the proper clinical context. X-ray should be considered in a trauma setting, for example to detect skull fractures. X-rays provide 2D images primarily used to see bones, tumors, and pneumonias. Computed tomography (CT) creates a 2D image which can help better visualize soft tissue and organs. CT without contrast is necessary to diagnose a subarachnoid hemorrhage or ischemic stroke. CT and X-rays are not without risks, there is small dose of radiation which can slightly increase the risk of cancer especially if the images add up over time. (14) Magnetic resonance imaging (MRI) offers a 2D image without radiation and is particularly useful to visualize the brain and spine, however it is not as readily available. While imaging can be useful it may also identify incidental findings which can lead to even more testing and patient anxiety. Choosing Wisely Canada in collaboration with the American College of Radiologists discourage the use of imaging unless red flags are present. (15)
Description of Primary Headaches:
When being presented with patients having headaches, the OPQRST mnemonic (onset, provocation, quality, radiation, severity, and time) will be especially important when assessing the type. A concise classification for the types of primary headaches are described and summarized in Table 2:
| Table 2: Primary headaches | Primary headache | Duration | Location | Pain intensity | Quality of pain | Associated symptoms |
| Migraine | 4-72 hours | Unilateral | Moderate | Pulsating | Nausea, vomiting, photophobia, Phonophobia |
| Tension-type | <4 hours | Bilateral (band-like fashion) | Moderate | Pressure | Migraine features notably absent |
| Cluster | <2 hours | Unilateral; orbital, supraorbital | Severe | Stabbing | Lacrimation, congestion, rhinorrhea, sweating, miosis, ptosis |
Migraines: predominantly unilateral in adults with a pulsating pain. Associated with nausea and sensitivity to sound or light. Often follow emotional stress, hormonal changes, physical exercises, irregular sleeping and eating patterns, or schedule changes. The duration can last from hours to days. Treatment includes ibuprofen, acetaminophen and amitriptylne. (16)
Tension headaches: episodic, occurring from one to multiple days a month. Bilateral pain described as tightness around the forehead with a fluctuating/pulsating intensity. Pain is not localized, nor severe. There is no aggravation by physical activity. The duration being 30 minutes to 7 days. Responds well with analgesia (ex, ibuprofen, or acetaminophen). (17)
Cluster: Unilateral pain around eye or temple. Symptoms involve the trigeminal nerve, including runny nose, Horner’s syndrome, sweating and pallor. Has a quick onset to a deep and excruciating pain. Lasts minutes to hours and occurs in cycles of a few days: hence, ‘cluster’. Acutely treated with 100% O2, and Triptans Prophylactic treatment may include verapamil, lithium and valproic acid. (18)
Beyond the Initial Approach
Management of primary headaches:
The management of primary headaches, specifically migraine headaches as seen in the patient above will be described. The management for secondary headaches involves treatment of the underlying cause.
Approximately half of patients that are treated for headaches will have a 50% reduction in headache frequency. (18) Recurrences are likely to occur in greater numbers due to the poor understanding of headache etiology and side effects of drugs leading to decreased compliance. While there is a high prevalence of headaches amongst the population there is no “one size fits all” approach. Having a patient-centered approach to treating headaches will result in a greater response to therapy.
The management of migraines can be divided into non-pharmacological and pharmacological types. The non-pharmacological treatments have moderate quality evidence in headache prevention and include proper sleep, stress management, and avoidance of triggers such as skipping meals, dietary (dark chocolate, red wine), excessive stress, and weather changes. (19)
Pharmacological treatment includes abortive and prophylactic choices. Abortive management is medication taken at the headache onset. First line therapy includes NSAIDs or acetaminophen. Second line includes triptans which are migraine specific. (19) While medication may work in the context of few headaches per month, medication-overuse headaches (MOH) are a serious concern in patients with higher frequency headaches. MOH can be triggered when abortive medication is taken greater than 9 days per month for triptans and 14 days per month with NSAIDs or acetaminophen. (20) In these patients, it is important to stop the medications and explore other avenues of treatments. Prophylactic management with low level evidence includes options such as vitamin B2 (riboflavin) and magnesium. (21) Other common options include tricyclic anti-depressants, beta-blockers and anticonvulsants (i.e., Topiramate or gabapentin) or anti-hypertensive agents (ARB or ACEi such as candesartan or lisinopril respectively). Certain aspects to consider are well-educating and reassuring the patient, medication side-effect profile, medication cost, patient values and preferences. With proper treatment and management, the frequency can be greatly reduced. It is worth noting that there is also an increased likelihood for patients with recurring headaches to have comorbid depression. (22) Thus, in addition to patient education concerning headaches, it is as important to provide patients with the proper tools and education to best look after their mental health
References
- Becker WJ, Findlay T, Moga C, Scott NA, Harstall C, Taenzer P. Guideline for primary care management of headache in adults. Can Fam Physician. 2015 Aug;61(8):670-9. PMID: 26273080; PMCID: PMC4541429. https://pubmed.ncbi.nlm.nih.gov/26273080/
- Latinovic R, Gulliford M, Ridsdale L. Headache and migraine in primary care: consultation, prescription, and referral rates in a large population. J Neurol Neurosurg Psychiatry. 2006 Mar;77(3):385-7. doi: 10.1136/jnnp.2005.073221. PMID: 16484650; PMCID: PMC2077680.
- Goadsby PJ, et al. Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiol Rev. 2017 Apr;97(2):553-622. doi: 10.1152/physrev.00034.2015. PMID: 28179394; PMCID: PMC5539409
- Strassman AM, Raymond SA, Burstein R. Sensitization of meningeal sensory neurons and the origin of headaches. Nature. 1996 Dec 12;384(6609):560-4. doi: 10.1038/384560a0. PMID: 8955268.
- Ahmed F. (2012). Headache disorders: differentiating and managing the common subtypes. British journal of pain, 6(3), 124–132. https://doi.org/10.1177/2049463712459691
- Ducros A, Bousser MG. Thunderclap headache. BMJ. 2013 Jan 8;346:e8557. doi: 10.1136/bmj.e8557. PMID: 23303883.
- Douglas, et al. Expert Panel on Neurologic Imaging. ACR Appropriateness Criteria® Headache. [Online Publication]. Reston (VA) American College of Radiology (ACR); 2013. Available at: https://acsearch.acr.org/docs/69482/Narrative/
- Richie MB, Josephson SA. A Practical Approach to Meningitis and Encephalitis. Semin Neurol. 2015 Dec;35(6):611-20. doi: 10.1055/s-0035-1564686. Epub 2015 Nov 23. PMID: 26595861.
- Klein AM, Loder E. Postpartum headache. Int J Obstet Anesth. 2010 Oct;19(4):422-30. doi: 10.1016/j.ijoa.2010.07.009. Epub 2010 Sep 15. PMID: 20833030.
- Chen, John J. MD, PhD; Bhatti, M. Tariq MD Papilledema, International Ophthalmology Clinics: Summer 2019 - Volume 59 - Issue 3 - p 3-22 doi: 10.1097/IIO.0000000000000274
- Wakerley BR. Medication-overuse headache. Pract Neurol. 2019 Oct;19(5):399-403. doi: 10.1136/practneurol-2018-002048. Epub 2019 Jul 4. PMID: 31273078.
- Rose JJ, Wang L, Xu Q, McTiernan CF, Shiva S, Tejero J, Gladwin MT. Carbon Monoxide Poisoning: Pathogenesis, Management, and Future Directions of Therapy. Am J Respir Crit Care Med. 2017 Mar 1;195(5):596-606. doi: 10.1164/rccm.201606-1275CI. Erratum in: Am J Respir Crit Care Med. 2017 Aug 1;196 (3):398-399. PMID: 27753502; PMCID: PMC5363978.
- Lagman-Bartolome AM, Gladstone J. Metabolic headaches. Neurol Clin. 2014 May;32(2):451-69. doi: 10.1016/j.ncl.2013.11.011. Epub 2014 Jan 11. PMID: 24703539.
- Miłowska K, Grabowska K, Gabryelak T. Zastosowanie promieniowania elektromagnetycznego w medycynie [Applications of electromagnetic radiation in medicine]. Postepy Hig Med Dosw (Online). 2014 May 8;68:473-82. Polish. doi: 10.5604/17322693.1101572. PMID: 24864099.
- Choosing Wisely. American College of Radiology: Five things physicians and patients should question
- Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018 Jan;38(1):1-211. doi: 10.1177/0333102417738202. PMID: 29368949.
- Burch R. Migraine and Tension-Type Headache: Diagnosis and Treatment. Med Clin North Am. 2019 Mar;103(2):215-233. doi: 10.1016/j.mcna.2018.10.003. Epub 2018 Dec 3. PMID: 30704678.
- Modi S, Lowder DM. Medications for migraine prophylaxis. Am Fam Physician. 2006 Jan 1;73(1):72-8. Erratum in: Am Fam Physician. 2006 Nov 15;74(10):1685. PMID: 16417067. https://pubmed.ncbi.nlm.nih.gov/16417067/
- Hainer BL, Matheson EM. Approach to acute headache in adults. Am Fam Physician. 2013 May 15;87(10):682-7. PMID: 23939446.
- Aleksenko D, Maini K, Sánchez-Manso JC. Medication Overuse Induced Headache. [Updated 2021 Jul 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK470171/
- Bianchi, A et al. (2004). Role of magnesium, coenzyme Q10, riboflavin, and vitamin B12 in migraine prophylaxis. Vitamins and hormones, 69, 297–312. https://doi.org/10.1016/S0083-6729(04)69011-X
- Beghi E, Bussone G, D’Amico D, Cortelli P, Cevoli S, Manzoni GC, Torelli P, Tonini MC, Allais G, De Simone R, D’Onofrio F. Headache, anxiety and depressive disorders: the HADAS study. The journal of headache and pain. 2010 Apr 1;11(2):141-50.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.