Approach to
Rotator cuff pathology
Courtenay Wood1
Published online: December 6, 2022
1McGill University
Corresponding Author: Courtenay Wood, email: courtenay.wood@mail.mcgill.ca
DOI: 10.26443/mjm.v21i1.957
Abstract
Shoulder pain is a common problem and the third most common musculoskeletal symptom for which patients seek medical care. Rotator cuff tendinosis is a frequent cause of this pain and can be diagnosed clinically with a careful history and physical exam. Treatment consists of a trial of pain management and physiotherapy and imaging modalities are often not required. However, imaging can be highly valuable for other pathologies. This article guides the reader through key elements to include in a history and physical exam of the shoulder, and how and when to select an appropriate imaging modality.
Tags: Rotator cuff tendinopathy, Shoulder pain, Imaging, Best practice
Question
You are a family medicine resident in a clinic. Your next patient is Mr. D, a 54-year-old accountant who enjoys playing baseball as a left-handed pitcher. He comes in with a 3-month history of insidious onset left shoulder pain.
He rubs the supero-lateral aspect of his deltoid as he describes a 5/10 diffuse pain that worsens with pitching, lifting objects, starting the lawn mower, and lying on that side. He has not tried any treatment for the pain. Mr. D denies weakness or limited range of motion. He denies shoulder injury and has had no previous surgeries or shoulder problems. His review of systems is unremarkable. He has a body mass index of 29 and has been diagnosed with hypertension and diabetes mellitus type 2 which are well-managed with Enalapril and metformin. Mr. D is otherwise in good health, and denies smoking, drinking or drug use.
In your physical exam, you do not note any asymmetry, swelling, erythema, atrophy or deformities in your thorough inspection and palpation of the shoulder. Mr. D has full active and passive range of motion of the shoulder. There is some tenderness in the musculature around the greater tubercle of the humerus and below the scapular spine.
You then perform a series of special orthopedic tests including the external and internal rotation resistance tests and the drop arm test. Mr. D does not demonstrate weakness when performing these tests but reports that it is painful to perform resisted external rotation.
What is the next best step in managing this patient?
- Plain radiographs of the shoulder
- Ultrasound (US)
- Magnetic resonance imaging (MRI)
- Magnetic resonance arthrography (MRA)
- 6-week trial of pain management physiotherapy
Answer
E. Mr. D’s case is typical of a rotator cuff tendinosis which usually does not require any imaging for diagnosis. In fact, there is a weak correlation between positive imaging findings and the presence of symptoms. (1) Management should include a 6-12 week trial of pain management, relative rest, and physiotherapy. (1, 2, 16) If symptoms do not improve after this trial, imaging modalities can then be considered and selected according to the patient’s history and physical exam findings.
Background
Problem
Shoulder pain is a common problem with a self-reported prevalence of 16-26% in the general population. It is the third most common musculoskeletal symptom for which patients seek medical care, followed by low back and knee pain.(3) Shoulder injury is associated with a delay in return to work and an increased frequency of sick leave.(4) Among the many etiologies of shoulder pain, rotator cuff (RC) disease - which includes tendinosis, impingement, and tears - is the most common.(5)
Anatomy
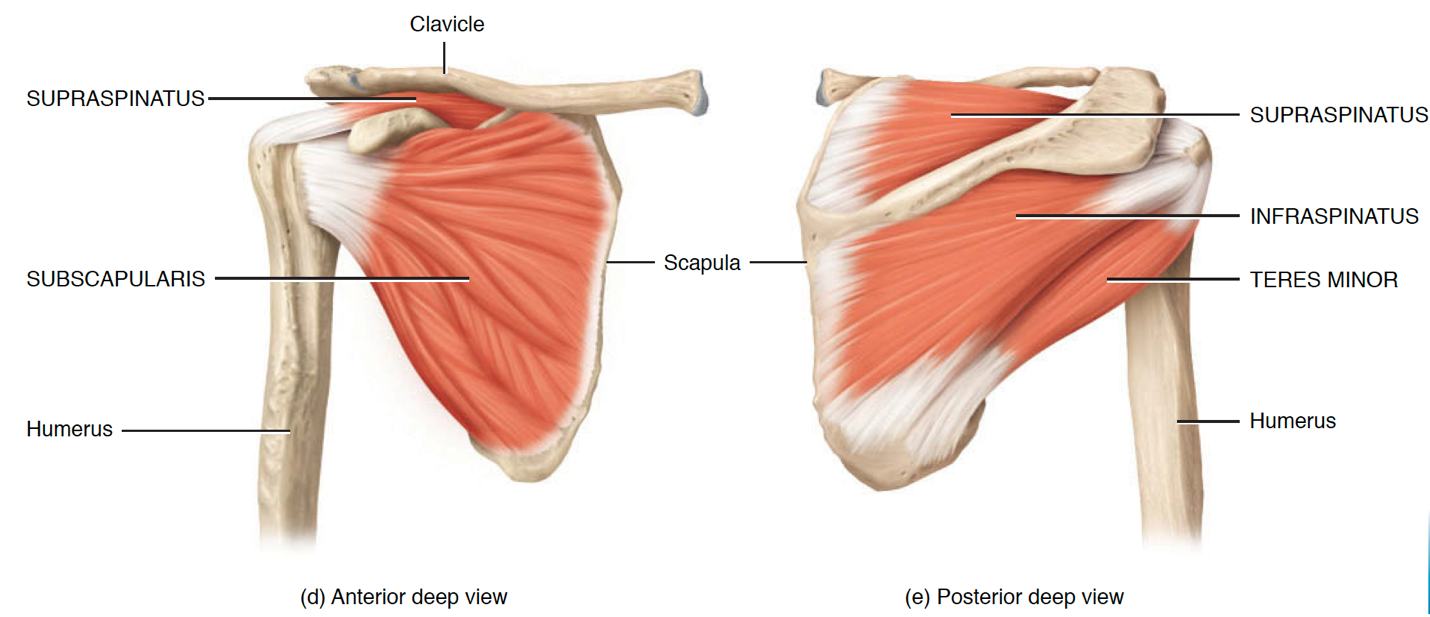
The RC includes the supraspinatus, infraspinatus, teres minor and subscapularis muscles. These muscles act as dynamic stabilizers of the glenohumeral joint.(5) The supraspinatus originates in the supraspinous fossa of the scapula, inserts on the greater tubercle of the humerus, and acts to abduct the shoulder. The infraspinatus and teres minor originate from the infraspinous fossa and inferior lateral border of the scapula, respectively, and both insert on the greater tubercle of the humerus. These muscles act to externally rotate the shoulder. Finally, the subscapularis originates from the subscapular fossa and inserts on the lesser tubercle of the humerus, acting to internally rotate the shoulder. See Figure 1 for the anatomy.(5)
A distinction must be made between RC tendinosis and RC tears as they may require different treatment. Tendinosis is treated with pain management and physical therapy.(1) However, in the case of a traumatic full-thickness RC tear, it is important to treat early with surgery. Untreated full-thickness tears may enlarge and the muscle may atrophy, predisposing the individual to recurrent tears.(3) Furthermore, if the tear becomes too large or is left too long without repair, intrinsic changes to the tendon may make it inoperable at a later date.(3)
Etiology of RC pathology
Multiple factors including over- or under-loading, age over 40 years, genetics, vascular changes, and an impinging acromion may lead to cumulative injury and degeneration which contribute to RC disease.(1, 6, 7, 9)
History
When taking the patient’s history, it is first important to determine whether there was any trauma to the shoulder as this will influence further management.(3, 12) Once trauma is ruled out, the physician must then ascertain whether the issue is indeed musculoskeletal in origin by doing a review of systems to rule out referred pain from other areas including the neck, diaphragm, gallbladder, and heart.
A detailed history on the nature and location of the pain will then help narrow down the diagnosis. RC tendinosis usually presents as atraumatic shoulder pain at the tip of the shoulder and supero-lateral aspect of the deltoid. The pain may worsen with activities such as reaching, punching, pulling, lifting, or lying on that side.(10) The presentation of a RC tear differs in that there may be weakness (e.g., with external rotation or abduction of the shoulder) in the affected muscle.(1, 10) Other examples of causes of non-traumatic shoulder pain include adhesive capsulitis, glenohumeral osteoarthritis, labral tears, biceps tendinopathy, avascular necrosis, and bone tumors.(8, 10)
Attention to risk factors for these shoulder pathologies should also be investigated. Risk factors that increase the likelihood of RC disease include: age, tissue over- or under-loading, an occupation or sport with overhead activity, diabetes mellitus, hypertension, high body mass index, and smoking.(1, 6)
Physical Examination
The physician should begin with observation of the patient.(12) They should note their posture, arm position, and the use of compensating accessory muscles. The physician should then inspect for swelling, erythema, atrophy, deformities, and any asymmetries between the shoulders and scapulae.(12) The physician should then proceed to palpate for any pain or deformities in the bony and muscular structures of the shoulder and surrounding joints. Next, they should assess the patient’s active and passive range of motion.(12)
Special orthopedic tests should then be employed to narrow down the diagnosis. Examples of these tests include the belly press test (sensitivity 28%, specificity 94%) and lift off test (sensitivity 19%, specificity 95%) for the subscapularis; Hornblower (sensitivity 17%, specificity 96%) for the infraspinatus; and Jobe’s test (sensitivity 88%, specificity 62%) and full can tests (sensitivity 7-% and sensitivity 81%), for the supraspinatus.(10, 12, 13) However, a combination of special orthopedic tests must be used to increase diagnostic accuracy (17) as none of these tests alone reliably isolate separate structures given their close proximity to one another.(1) Normal strength in a series of tests may point the physician toward a tendinosis whereas weakness may allow the physician to diagnose a RC tear.(1, 12, 14)
Treatment for RC tendinosis
Pain management
Adequate pain management and a prompt return to work are important components of the recovery process.(2, 15) Non-pharmacological measures such as ice, heat, and massage as well as pharmacological agents including acetaminophen or nonsteroidal anti-inflammatory drugs should be employed for pain relief.(2, 15) If these pain management measures plus exercise programs are not effective in relieving pain, cortisone or local anesthetic injections may provide some temporary analgesia.(1, 2, 17)
Physical therapy
Fortunately, RC tendinosis can be managed with physical therapy which has a 75% success rate.(16) These exercise programs include three stages: shoulder mobility, building strength and flexibility, and integration towards sports or occupation-specific activities such as a return-to-work program.(15, 18) Pain and function usually improve after just 6 to 12 weeks of a rehabilitation exercise program.(16) Treatment should involve relative rest from or modification of painful activities, adjusting posture, avoiding sleeping on the sore shoulder, controlled reloading, sustained isometric contractions, and progression from simple to complex shoulder movements.(1, 2) Compared with surgery, this rehabilitative approach brings the additional benefit of implementing exercise, minimizing sick leave with a faster return to work, and reducing costs to the healthcare system.(1) Likewise, for non-traumatic partial thickness tears, surgery has no better outcome than an exercise program.(1, 17) In fact, exercise programs are beneficial even in large inoperable RC tears.(1, 17)
However, despite the benefits of exercise, surgery may still be warranted in traumatic, full-thickness tears as there is a risk that the size of the tear, fatty infiltration and muscle atrophy may all increase over time(3,6). Without prompt surgery on these acute tears, the tissue may be inoperable and unable to recover with conservative management.(3)
Beyond the Initial Approach
Imaging
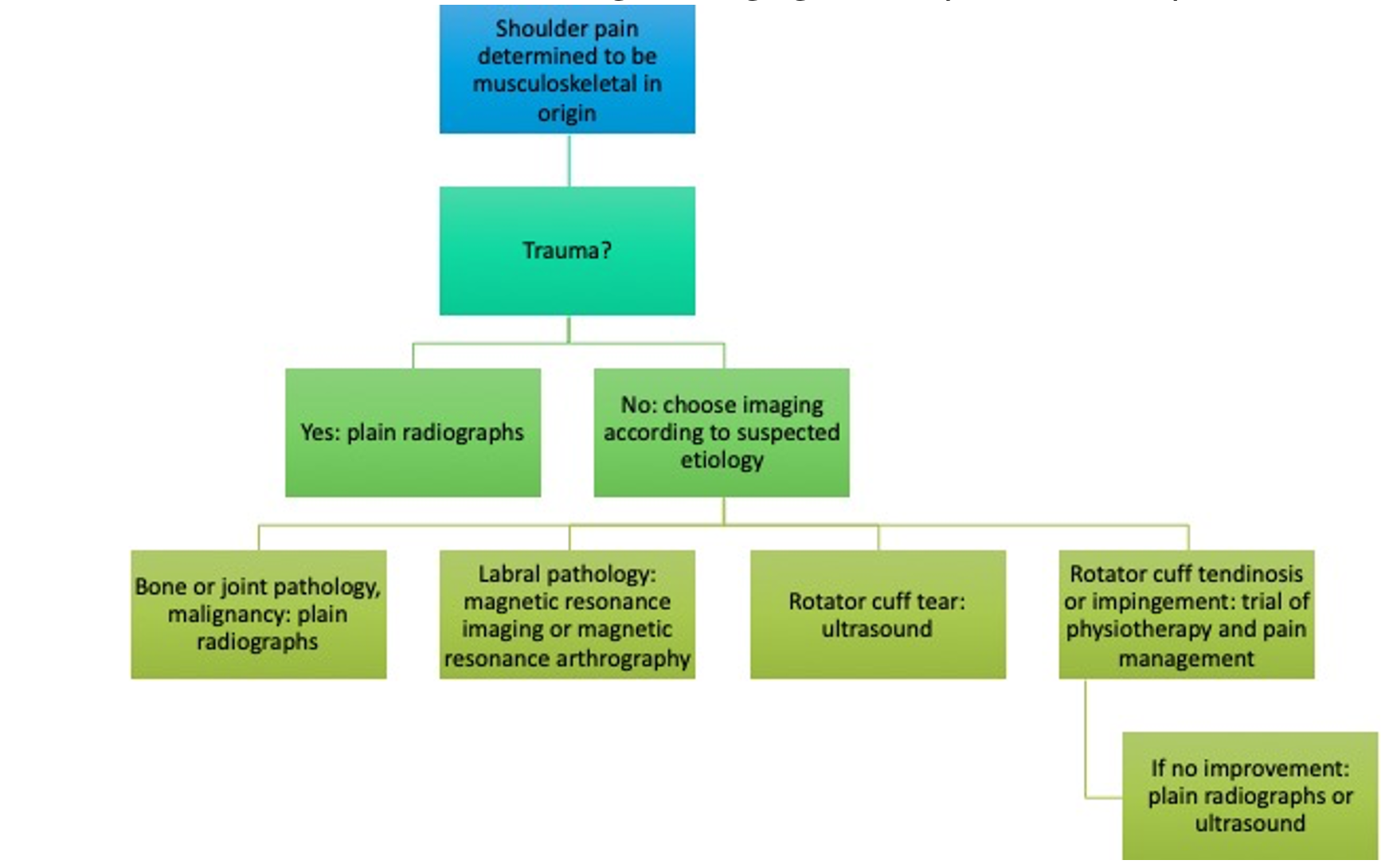
Although imaging can be a critical diagnostic tool for shoulder pathologies, it must be used wisely and the modality must be chosen carefully based on the patient’s history and physical exam findings.(3) With RC tendinosis in particular, there is a very weak association between symptoms and structural changes found on imaging, which challenges the validity of using imaging to justify that structural abnormalities lead to pain in RC tendinosis.(1) See Flow Chart 1 for a decision tree regarding selection of imaging modalities.
Utility of plain radiographs
Although plain radiographs of the shoulder may not be necessary in the initial investigation of non-traumatic shoulder pain, they should be the first imaging modality in acute trauma, especially given their ease of access and low cost.(19) X-rays can provide information about pathologies such as fractures, osteoarthritis, malignancy, dislocation, Hills-Sachs lesions, and Bennett Lesions to name a few.(3, 9, 14, 19) Although plain radiographs can also detect abnormalities related to impingement, such as osteophyte formation or a down sloping acromion, these findings are commonly present in asymptomatic patients as well and must be interpreted with caution.(9, 14)
Utility of US, MRI, and MRA
Since chronic partial RC tears and tendinosis are treated similarly, whereas acute traumatic full thickness tears may require timely surgery for the best prognosis, it is most important to choose a modality that can accurately detect a full-thickness tear in a timely manner.(3, 11) US, MRI, and MRA perform equally well in the detection of full-thickness tears.(3, 11) Ultrasound should be the first-line imaging of choice over MRI or MRA given its low cost, portability, availability, real-time imaging, short scan times, and greater patient satisfaction. Furthermore, MRI and MRA have contraindications such as metal implants or claustrophobia, which ultrasound avoids.(3, 9, 11, 19) If ultrasound imaging remains inconclusive, the patient should then undergo MRI or MRA.(3)
Although ultrasound carries the above benefits, it does have some shortcomings. One major disadvantage of ultrasound is the necessity of personnel trained in ultrasound imaging of the RC.(19) When it comes to evaluating partial thickness tears, MRA may be the best imaging modality for this pathology given its superior sensitivity compared to US or MRI.(11) Finally, ultrasound has a limited ability to provide information about labrum, ligamentous, and osseous abnormalities;(3, 9) here, MRI or MRA would be the first-line imaging choice,(3) especially in younger populations less than 40 years of age where labral injuries are more common.(9)
Summary
RC disease is the most common etiology of shoulder pain and includes a continuum of pathologies including tendinosis, tears, and impingement. RC disease can often be diagnosed clinically with a history and physical exam.(1) In the case of traumatic full thickness tears, prompt surgery is recommended.(3) For tendinosis, if symptoms do not improve after a 6-12 week (16) course of conservative treatment, imaging may be indicated. The modality of choice should be carefully selected based on the suspected etiology according to the patient’s presentation. In general, plain radiographs are best used to assess bone and joint pathology, ultrasound is best for RC or bursal pathology, and MRI or MRA are best for labral pathology.(20)
Flow Chart, Figures, Tables, & Legends
References
- Lewis J, McCreesh K, Roy JS, Ginn K. Rotator cuff tendinopathy: navigating the diagnosis-management conundrum. Journal of orthopaedic & sports physical therapy. 2015 Nov;45(11):923-37. Available from: doi:10.2519/jospt.2015.5941
- Doiron-Cadrin P, Lafrance S, Saulnier M, Cournoyer É, Roy JS, Dyer JO, Frémont P, Dionne C, MacDermid JC, Tousignant M, Rochette A. Shoulder rotator cuff disorders: a systematic review of clinical practice guidelines and semantic analyses of recommendations. Archives of physical medicine and rehabilitation. 2020 Jul 1;101(7):1233-42. Available from: doi:10.1016/j.apmr.2019.12.017
- Nazarian LN, Jacobson JA, Benson CB, Bancroft LW, Bedi A, McShane JM, Miller TT, Parker L, Smith J, Steinbach LS, Teefey SA. Imaging algorithms for evaluating suspected rotator cuff disease: Society of Radiologists in Ultrasound consensus conference statement. Radiology. 2013 May;267(2):589-95. Available from: doi: 10.1148/radiol.13121947
- Desmeules F, Braen C, Lamontagne M, Dionne CE, Roy JS. Determinants and predictors of absenteeism and return-to-work in workers with shoulder disorders. Work. 2016 Jan 1;55(1):101-13.
- Tortora, GJ, & Derrickson, B. Principles of anatomy and physiology. 14th ed. Danvers, MA: Wiley; c2014
- Weber S, Chahal J. Management of rotator cuff injuries. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2020 Mar 1;28(5):e193-201.
- Thomopoulos S, Parks WC, Rifkin DB, Derwin KA. Mechanisms of tendon injury and repair. Journal of Orthopaedic Research. 2015 Jun;33(6):832-9. Available from doi:10.1002/jor.22806
- Ponnappan RK, Khan M, Matzon JL, Sheikh ES, Tucker BS, Pepe MD, Tjoumakaris FP, Nassr AN. Clinical differentiation of upper extremity pain etiologies. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2015 Aug 1;23(8):492-500.
- Yablon CM, Jacobson JA. Rotator cuff and subacromial pathology. Seminars in musculoskeletal radiology. 2015 Jul;19(03):231-242. Available from: doi:10.1055/s-0035-1549317
- Anderson BC. Office orthopedics for primary care: diagnosis. Elsevier Health Sciences; 2005 Dec 7.
- Roy JS, Braën C, Leblond J, Desmeules F, Dionne CE, MacDermid JC, Bureau NJ, Frémont P. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. British journal of sports medicine. 2015 Oct 1;49(20):1316-28. Available from: doi:10.1136/bjsports-2014-094148
- Reider B. The Orthopedic Physical Examination. 2nd ed, Philadelphia PA: Elsevier Saunders; c2005.
- Jain NB, Luz J, Higgins LD, Dong Y, Warner JJ, Matzkin E, Katz JN. The diagnostic accuracy of special tests for rotator cuff tear: the ROW cohort study. American journal of physical medicine & rehabilitation. 2017 Mar;96(3):176.
- Harrison AK, Flatow EL. Subacromial impingement syndrome. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2011 Nov 1;19(11):701-8.
- Hopman K, Krahe L, Lukersmith S, McColl AR, & Vine K. Clinical Practice Guidelines for the Management of Rotator Cuff Syndrome in the Workplace. The University of New South Wales; c2013. Available at: https://rcs.med.unsw.edu.au/sites/default/files/rcs/page/RotatorCuffSyndromeGuidelines.pdf
- Kuhn JE, Dunn WR, Sanders R, An Q, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Holloway BG, Jones GL, Ma CB. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. Journal of shoulder and elbow surgery. 2013 Oct 1;22(10):1371-9.
- American Academy of Orthopaedic Surgeons. Management of Rotator Cuff Injuries Evidence- Based Clinical Practice Guideline. Rosemont (IL): American Academy of Orthopaedic Surgeons; 2019 Mar 11 [cited 2022 Jan 29]. Available from: https://www.aaos.org/globalassets/quality-and-practice-resources/rotator-cuff/rotator-cuff-cpg-final-12-20-19.pdf.
- Krabak BJ, Sugar R, McFarland EG. Practical nonoperative management of rotator cuff injuries. Clinical Journal of Sport Medicine. 2003 Mar 1;13(2):102-5.
- Anderson MW, Brennan C, Mittal A. Imaging evaluation of the rotator cuff. Clinics in sports medicine. 2012 Oct 1;31(4):605-31. Available from: doi:10.1016/j.csm.2012.07.010
- Canadian Academy of Sport and Exercise Medicine. Recommendations: Sport and Exercise Medicine. Choosing Wisely Canada [internet]; 2021 Sep [cited 2022 Jan 29]. Available from https://choosingwiselycanada.org/sport-exercise-medicine/

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.