Approach to
Concussion in the Adult Athlete
Laurence Désilets-Barnabé1 and Philippe Moisan2
Published online: October 23, 2021
1Université de Montréal
2McGill University
Corresponding Author: Laurence Désilets-Barnabé, email: laurence.desilets-barnabe@umontreal.ca
DOI: 10.26443/mjm.v21i1.945
Abstract
Concussions are common in the athlete population. They occur after a trauma to the head and can lead to a loss of consciousness. Patients suffering from a concussion commonly present with confusion, amnesia and a headache in the context of a recent head trauma. The approach to this pathology consists in making a clinical diagnosis, ruling out life-threatening complications such as fractures and intracranial hemorrhages and educating the patient on a safe recovery and return-to play. Patients that do not have worrisome symptoms can be discharged home with a responsible adult that has been informed of when to seek medical care in case of a complication. After a short rest period they should be advised to resume gradually their cognitive and physical activity. After a minimal period of 10 days and in the absence of symptoms, the patients can undergo a progressive return to play plan.
Tags: Sport medicine, concussion, return to play, athlete, traumatic brain injury.
Question
A 22-year-old soccer player presents to the emergency room complaining of a headache after being accidentally hit in the head by a ball during practice. He describes feeling the ball hit the side of his head and falling immediately on the ground after the impact. He denies losing consciousness. On further questioning, he has no past medical history, takes no medications, but recalls a similar event happening two years ago that forced him to miss school for two weeks due to headaches and difficulty focusing in class. On physical examination, there is a 3 × 2 cm mildly tender ecchymosis on the side of his head. Neurological examination shows mildly impaired attention but is otherwise normal.
After making the diagnosis, what recommendations should be made to this patient?
- Stop all contact sports to avoid another concussion.
- Full cognitive and physical rest for at least two weeks after the injury.
- Avoid non-steroidal anti-inflammatory (NSAID) medications for 7–10 days due to the risk of intracranial bleeding.
- Rest for 24–72 hours before resuming non-contact physical activity as tolerated.
Answer
D. Rest for 24–72 hours before resuming non-contact physical activity as tolerated
The correct answer is to resume physical activity gradually after a short period of physical and cognitive rest. Patients should not be told to stop all contact sports but a discussion with the family should be had to reduce the risk of additional injuries. NSAIDs are first-line medications for treating post-concussion headaches. Prolonged cognitive and physical rest has been shown to slow the recovery and lead to longer post-concussion symptoms. Persistent post-concussive symptoms (PPCS) are defined by symptoms lasting longer than the natural post-injury course. Patients with PPCS may present clusters of vestibulo-ocular, cervicogenic, migrainous and psychological symptoms. (1)
Overview of Conussions
What is a concussion?
Concussions, also called mild traumatic brain injury (mTBI) are a common medical condition in both the athlete and the general population. Concussions may be caused by a direct blow to the head or by any force on another part of the body that is transmitted to the head. Many definitions of concussion exist as there are multiple mechanisms of injury and a large range of symptoms associated with concussions. The American Academy of Neurology defined concussions as “a clinical syndrome of biomechanically induced alteration of brain function typically affecting memory and orientation, which may involve loss of consciousness.” (2) Although not fully elucidated, the pathophysiology includes a sudden release of excitatory neurotransmitters inducing a glycolytic hypermetabolic state and lactate production which impairs neuronal function. (3)
Epidemiology
Approximately 1.2% of the Canadian population sustain a mTBI every year. (4) The prevalence of mTBI varies depending on the population observed. In the general population, men are at least two times more likely to sustain a concussion than women. (5, 6) However, women are more likely to sustain a mTBI while playing sports, regardless of their level. (7) The sports most associated with mTBI are football, ice hockey, soccer, boxing, and rugby. (8) It is common for athletes to refuse disclosing a potential concussion. These situations are dangerous as they increases the risk of second impact syndrome. (9) Second impact syndrome is defined as a second brain trauma occurring on a previously injured brain that has not fully recovered.(10) Although not fully understood, it is postulated that it results in a rapid brain swelling that can lead to herniation and catastrophic neurological damage.(11)
Initial Approach
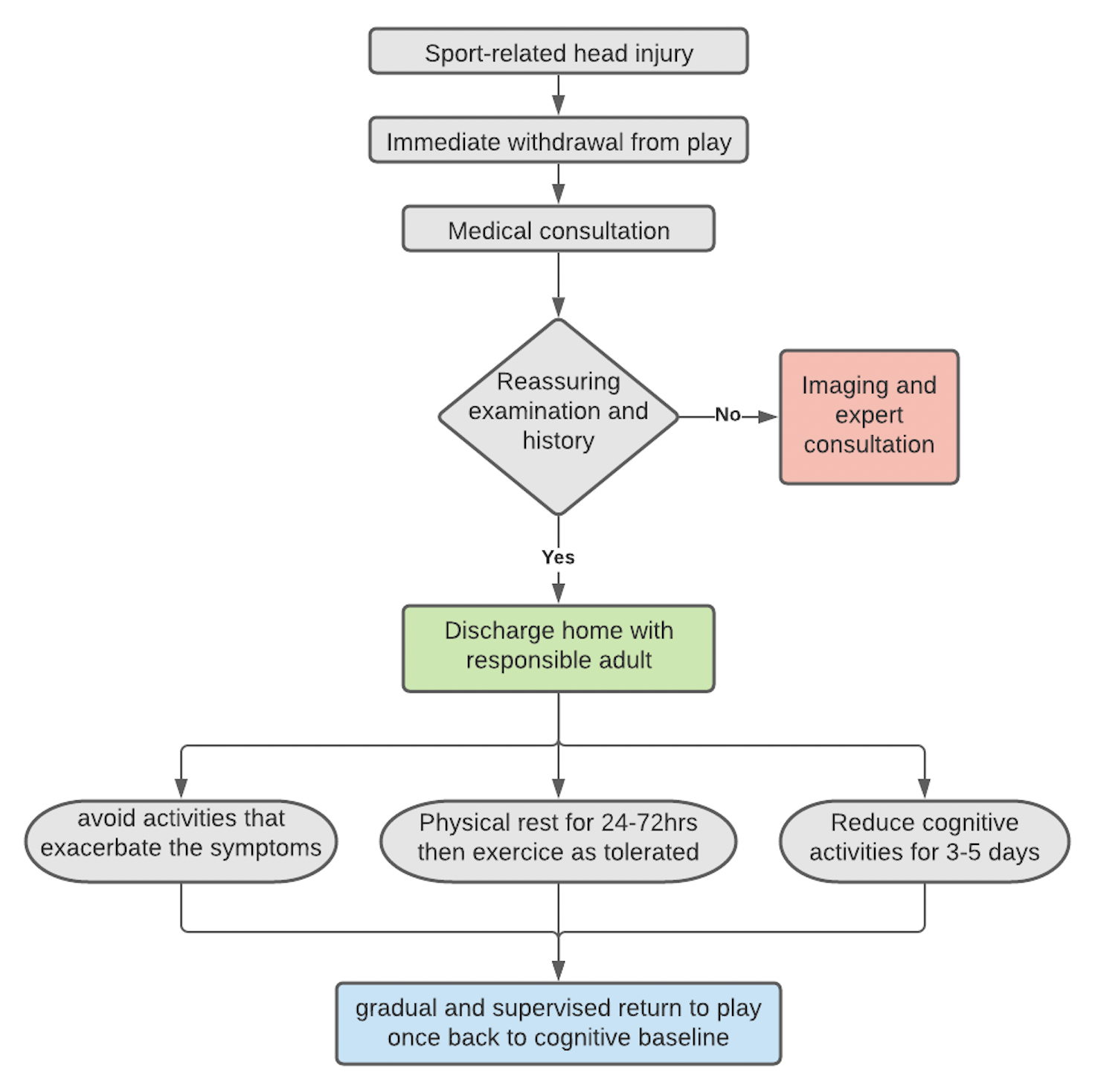
The goals of the initial approach to this condition are to make the diagnosis, rule out life-threatening conditions with additional tests when indicated, and to advise the patient on behaviour modification and recovery strategies.
Clinical Presentation and Diagnosis
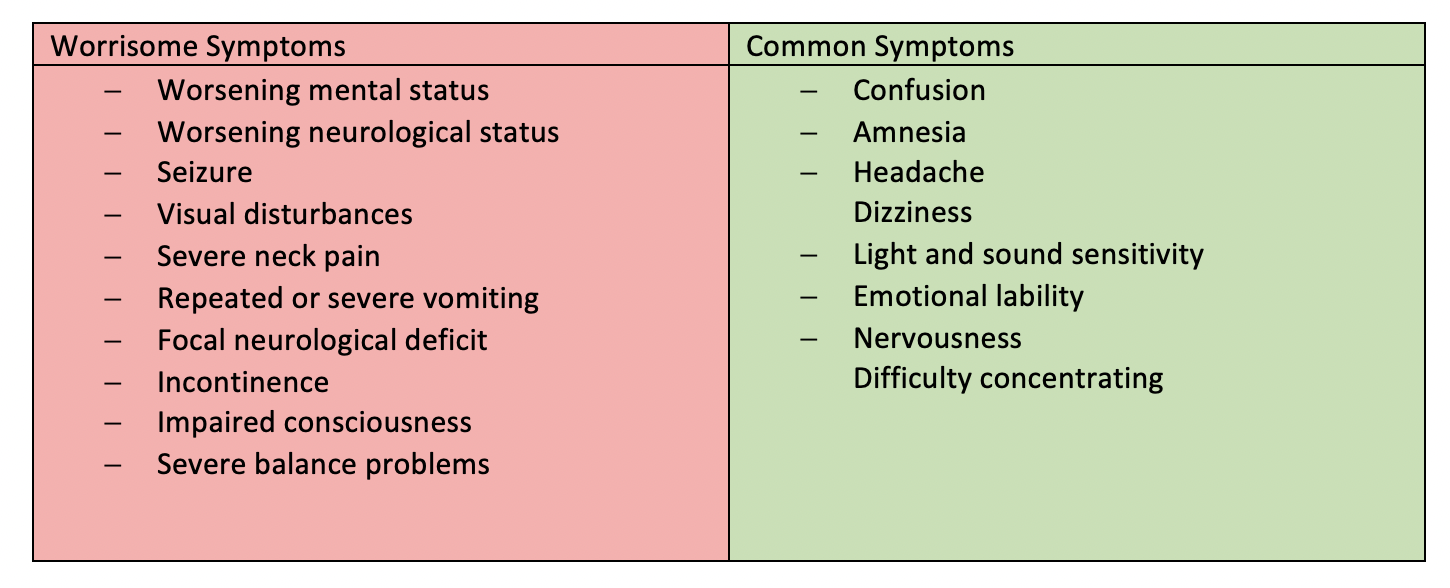
Signs and symptoms of a concussion may take up to 48 hours to manifest. The hallmark symptoms of concussion are confusion and amnesia. (12, 13) Other common symptoms include new or worsening difficulty thinking or concentrating, new or worsened headaches, dizziness, light and sound sensitivity, and emotional symptoms such as nervousness and emotional lability. (14) (Table 1) The diagnosis of mTBI is clinical.
Many tools are available to assess concussions. They can be categorized as screening and confirmatory tools. (15) The most common screening tools are the Standardized Assessment of Concussion (SAC). Screening tools can be used to assess the risk of concussion immediately after an injury to remove an athlete from the game. Other tools, such as the SCAT5 (Sport Concussion Assessment Tool 5th Edition) and the impact (immediate post-concussion assessment and cognitive testing), are more extensive and used in a clinical settings as they provide a more in-depth assessment of the athlete’s condition and allow follow-up testing. The SCAT5 is the most common validated tool that can assist the clinician in diagnosing a concussion in the acute setting. This evaluation tool combines a symptom evaluation, cognitive and gross neurological function assessment. It has been demonstrated as especially useful before the 3-5 days post injury to aid in the diagnosis. (16)
The physician must take a complete history, physical and neurological examination to associate a head trauma with an above-mentioned symptom and make the diagnosis. On history it is essential for the physician to clearly understand the mechanism of injury to determine the severity of the head and associated injuries. Some factors associated with a more severe injury are high speed or high energy injuries – where the brain could be exposed to a greater force of impact inside the cranium. Whiplash injuries are associated with cervical and vestibular injuries in addition to brain injuries. (17) The patients should be questioned on previous head injuries (including possible undiagnosed concussions), medication use (particularly medications that increase the risk of bleeding) and associated injuries such a neck or back pain. At any time if an injury to the cervical spine is suspected, the patient should be immobilized until a fracture can be ruled out.
The physical examination should be focused on identifying fractures, cerebrospinal fluid leaks and other injuries. To do so, the physician should carefully palpate the patient’s head, look for otorrhea or rhinorrhea and complete a head-to-toe examination to rule out other injuries. A complete neurological examination should be done on the first assessment. It should include a baseline mental status exam, cognitive assessment, and a thorough examination of the cranial nerves. It should also look for neurological deficits and signs of increased intracranial pressure such as headache, vomiting and visual changes. Acute and mild impairment in cognition might be normal but focal neurological deficits, worsening neurological status or mental status are worrisome features that warrant further investigation. Laboratory tests and imaging are not routinely used but might be useful when life-threatening complications such as fractures of intracranial bleed are suspected.
Complications
Most mTBI are uncomplicated, but 6–10% are associated with cerebral contusions that can lead to intracerebral, subdural, epidural or subarachnoid hemorrhages. (18) It is essential for the physician to recognize these complications rapidly since they can be life-threatening and are associated with a poor functional prognosis. (19)
Worrisome symptoms that warrant urgent imaging are a suspicion of fractures, worsening neurological status, worsening level of consciousness, cerebrospinal fluid otorrhea or rhinorrhea, severe headaches, repeated vomiting, and seizures (Table 2). If a bleed or fracture is suspected, the patient should receive an urgent computed tomography (CT) of the head without contrast and be referred to a neurosurgeon.
Treatment
The treatment of an uncomplicated sport-related concussion consists of outpatient observation if the patient has a Glasgow coma scale (GCS) of 15, which indicates intact cognitive function (the patient is responsive with optimal eye, verbal and motor responses), a normal examination or CT and no risk factors for bleeding such as anticoagulation, or a genetic disorder. (20) After possible complications and life-threatening conditions have been ruled out, the patient can be discharged home if accompanied and supervised by a responsible adult. It is essential to educate the patient and their caregiver on when and how to seek medical attention if a complication occurs. Parents should seek immediate attention if there is a change in the mental status, level of arousal, significant increase in headache, or visual changes.
Symptoms such as impaired attention, difficulty concentrating and sleepiness will improve with time. Post-concussive headache symptoms can be managed effectively with simple analgesics such as NSAIDs. If not effective, triptans can be used for headaches with migrainous features. (3) Multiple new treatment modalities are currently being studied. Transcranial pulsating low-frequency electromagnetic stimulation (21) and hyperbaric oxygen therapy (22) has been studied in small groups of patients with long-lasting concussion symptoms.
Beyond the Initial Approach
Patient Counselling
Traditional advice was to avoid all physical and cognitive activities for a prolonged period after a concussion. It has been demonstrated that moderate cognitive activity is equivalent to complete cognitive rest. (23) Patients should be advised to reduce significantly their cognitive activity for 3–5 days after the injury and then scale up as tolerated. (3) Contrary to previous advice, recent studies have shown that early physical activity following a concussion is beneficial and leads to lower rates of persistent post-concussive symptoms. Patients should be advised to rest for 24–72 hours and then exercise as tolerated. (3, 14) The goal is that following a short period of rest, patients should gradually reintegrate cognitive and physical activity without exacerbating their symptoms.
Returning to Sport Following a Concussion
Return to sport following a concussion should be gradual and may vary upon the injury sustained by the patient. For a uncomplicated sport-related injury, the athlete should not engage in physical activity for the first 48 hours following the concussion. After 48 hours post-injury, the patient may gradually return to physical and intellectual activities. This gradual return to activities has multiple steps separated by a minimum of 24 hours. To progress to the next step, the patient needs to be able to complete the activity without an increase in the number or intensity of their symptoms. If symptomatic, the patient needs to wait another 24 hours and return to the previous step. (24) A concussed player should only return to high-intensity training (with or without the team) once there has been a complete return to normal cognitive activities such as school or work. (24) To reduce the risks of second-impact syndrome which can be catastrophic (25) patients should not undergo any activities that put them at risk of head injury before a minimum of 10 days after the injury. (3, 26)
References
- Cara MP, Ricardo J. Fernández-de T, Andrew l. S. Postconcussive Syndrome. 2022.
- Christopher CG, Jeffrey SK, Stephen A, Jeffrey B, Thomas SDG, Gerard AG, et al. Summary of evidence-based guideline update: Evaluation and management of concussion in sports. 2013.
- Mullally W. Concussion. The American journal of medicine. 2017;130(8).
- Langer L, Levy C, Bayley M. Increasing Incidence of Concussion: True Epidemic or Better Recognition? The Journal of head trauma rehabilitation. 2020;35(1).
- Feigin V, Theadom A, Barker-Collo S, Starkey N, McPherson K, Kahan M, et al. Incidence of traumatic brain injury in New Zealand: a population-based study. The Lancet Neurology. 2013;12(1).
- Kraus J, McArthur D. Epidemiologic aspects of brain injury. Neurologic clinics. 1996;14(2).
- Delaney J, Lacroix V, Leclerc S, Johnston K. Concussions among university football and soccer players. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2002;12(6).
- Guerriero R, Proctor M, Mannix R, Meehan W. Epidemiology, trends, assessment and management of sport-related concussion in United States high schools. Current opinion in pediatrics. 2012;24(6).
- Kerr Z, Register-Mihalik J, Marshall S, Evenson K, Mihalik J, Guskiewicz K. Disclosure and non-disclosure of concussion and concussion symptoms in athletes: review and application of the socio-ecological framework. Brain injury. 2014;28(8).
- McLendon LA, Kralik SF, Grayson PA, Golomb MR. The Controversial Second Impact Syndrome: A Review of the Literature. Pediatr Neurol. 2016;62:9-17.
- McCrory P, Meeuwisse W, Aubry M, Cantu B, Dvorák J, Echemendia R, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. British journal of sports medicine. 2013;47(5).
- Practice parameter: the management of concussion in sports (summary statement). Report of the Quality Standards Subcommittee. Neurology. 1997;48(3).
- Duhaime A, Beckwith J, Maerlender A, McAllister T, Crisco J, Duma S, et al. Spectrum of acute clinical characteristics of diagnosed concussions in college athletes wearing instrumented helmets: clinical article. Journal of neurosurgery. 2012;117(6).
- Silverberg ND, Division of Physical Medicine & Rehabilitation UoBC, Vancouver, British Columbia, Canada, Rehabilitation Research Program GSRC, Vancouver, British Columbia, Canada, Duhaime A-C, Neurosurgery MGH, Neurosurgery, Harvard Medical School, Boston, Iaccarino MA, et al. Mild Traumatic Brain Injury in 2019-2020. JAMA. 2021;323(2):177-8.
- Kaufman M, Su C, Trivedi N, Lee M, Nelson G, Cupp S, et al. The Current Status of Concussion Assessment Scales: A Critical Analysis Review. JBJS reviews. 2021;9(6).
- Echemendia R, Meeuwisse W, McCrory P, Davis G, Putukian M, Leddy J, et al. The Sport Concussion Assessment Tool 5th Edition (SCAT5): Background and rationale. British journal of sports medicine. 2017;51(11).
- Rebbeck T, Evans K, Elliott J. Concussion in Combination With Whiplash-Associated Disorder May Be Missed in Primary Care: Key Recommendations for Assessment and Management. The Journal of orthopaedic and sports physical therapy. 2019;49(11).
- Wintermark M, Sanelli P, Anzai Y, Tsiouris A, Whitlow C. Imaging evidence and recommendations for traumatic brain injury: conventional neuroimaging techniques. Journal of the American College of Radiology : JACR. 2015;12(2).
- Hsiang J, Yeung T, Yu A, Poon W. High-risk mild head injury. Journal of neurosurgery. 1997;87(2).
- Jagoda A, Bazarian J, Bruns J, Cantrill S, Gean A, Howard P, et al. Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Annals of emergency medicine. 2008;52(6).
- Miller C, Prener M, Dissing S, Paulson O. Transcranial low-frequency pulsating electromagnetic fields (T-PEMF) as post-concussion syndrome treatment. Acta neurologica Scandinavica. 2020;142(6).
- Harch P, Andrews S, Rowe C, Lischka J, Townsend M, Yu Q, et al. Hyperbaric oxygen therapy for mild traumatic brain injury persistent postconcussion syndrome: a randomized controlled trial. Medical gas research. 2020;10(1).
- Brown N, Mannix R, O'Brien M, Gostine D, Collins M, Meehan W. Effect of cognitive activity level on duration of post-concussion symptoms. Pediatrics. 2014;133(2).
- Québec Gd. Protocole de gestion des commotions cérébrales. In: supérieur mdlÉedlE, editor. 2019.
- May T, Foris L, Donnally IC. Second Impact Syndrome. 2021.
- McCrory P, Davis G, M M. Second impact syndrome or cerebral swelling after sporting head injury. Current sports medicine reports. 2012;11(1).

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.