Approach To
Acute Kidney Injury
Sophy Mo1
Published online: January 25 2022
1Faculty of Medicine, McGill University, Montreal, QC, Canada
Corresponding Author: Sophy Mo, sophy.mo@mail.mcgill.ca
DOI: 10.26443/mjm.v20i2.943
Abstract
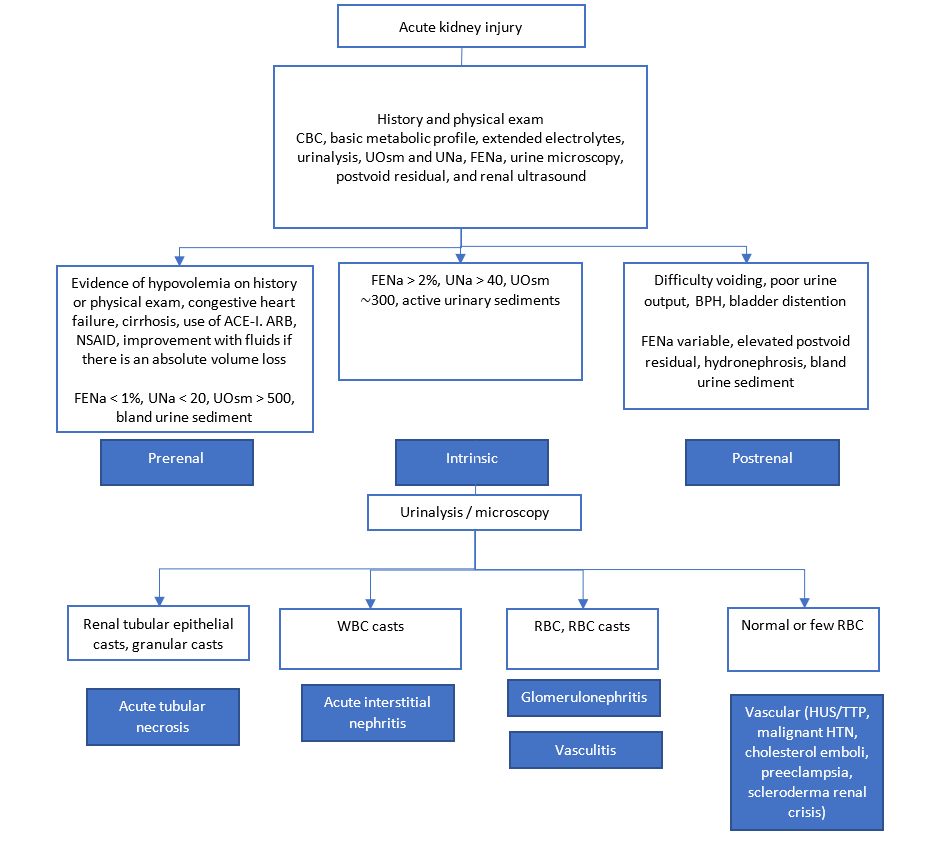
Acute kidney injury is defined as an abrupt decline in kidney function, which manifests as an increase in serum creatinine level or a decrease in urine output within a short period of time. It is a commonly encountered entity in the clinical setting and necessitates a systematic diagnostic approach. Acute kidney injury etiologies are classified as either prerenal, intrinsic renal, or postrenal. This article presents the key elements of history taking, physical examination, and laboratory investigations when assessing a patient for acute kidney injury to properly classify its etiology. The use of imaging modalities is also discussed. Common etiologies of acute kidney injury in each category are highlighted. Lastly, this article provides a brief overview of management principles for acute kidney injury with a particular emphasis on indications for initiation of dialysis.
Tags: Acute kidney injury, Acute tubular necrosis, Creatinine, Renal failure, Urine microscopy.
Question
A 39-year-old female presents to the emergency department at the request of her family physician due to a 2-day history of vomiting and profuse diarrhea. She returned from a cruise yesterday and recalls other travelers were sick on the cruise. She is known for anxiety, gastroesophageal reflux, and patellofemoral syndrome. Her prescribed medications are sertraline and ranitidine. On history, she reports feeling well until two days ago. Since then, she has been vomiting and having diarrhea incessantly. She also had very little appetite and has not been eating or drinking well. She has been mostly staying in bed and reports some dizziness when standing up to go to the bathroom. She saw her family doctor yesterday, who obtained blood tests. Notably, her creatinine level was 135 $μmol/L. Three months ago, her creatinine level was 67 μmol/L on routine blood work.
Which of the following physical examination findings is not consistent with your suspected cause of acute kidney injury?
A. Absence of crackles on lung exam
B. Orthostatic hypotension
C. Distended bladder
D. Low jugular venous pressure
E. Postural tachycardia
Answer
C. This patient’s history is suggestive of a prerenal acute kidney injury in the context of significant dehydration. Indications of this etiology include poor oral intake and significant fluid loss from vomiting and diarrhea. The patient also complains of dizziness upon standing, which reflects orthostatic hypotension secondary to hypovolemia. On physical examination, she would be expected to have findings consistent with hypovolemia, which include absence of crackles on lung exam (A), orthostatic hypotension (B), low jugular venous pressure (D), and postural tachycardia (E). A distended bladder is more consistent with postrenal acute kidney injury, which is commonly due to benign prostatic hyperplasia in older men. It is not a finding that would be associated with prerenal acute kidney injury.
Initial Approach
Diagnosis
Acute kidney injury (AKI) is defined as any of the following: 1. Increase in serum creatinine ≥26.5 μmol/L within 48 hours; or 2. Increase in serum creatinine ≥1.5 times the baseline, which is known or presumed to have occurred within the prior 7 days; or 3. Urine volume <0.5 mL/kg/h for 6 hours (1). It is important to distinguish between AKI and chronic kidney disease (CKD). Hence, a recent creatinine level indicating the patient’s baseline is especially useful. When it is not available, CKD is suspected based on certain laboratory findings (e.g., normocytic anemia, elevated parathyroid hormone) and radiologic findings (e.g., small, shrunken kidneys with cortical thinning). AKI on CKD is also very common. Therefore, measuring the serum creatinine over several days may be needed to document an AKI (2).
History taking
The patient’s history often provides important clues regarding the cause of AKI: prerenal, postrenal, or intrinsic.
Prerenal AKI results from poor renal perfusion. It is often associated with an absolute volume loss, which can be suggested by a history of poor fluid intake or fluid loss such as vomiting or diarrhea (2). An improvement of the AKI after fluid resuscitation is indicative of this cause for the prerenal AKI (3). Certain medical conditions such as congestive heart failure, cirrhosis, and sepsis can also result in poor renal perfusion resulting in prerenal AKI. Lastly, specific medications are associated with prerenal AKI due to their effect on the afferent and efferent arterioles. These include angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and nonsteroidal anti-inflammatory drugs (4).
Postrenal AKI results from the obstruction of the urinary flow anywhere from the kidney to the urethra. When the obstruction is above the bladder, it usually must affect both kidneys to result in significant AKI. The patient may complain about difficulty voiding and poor urine output (1). Benign prostatic hyperplasia is a common cause in older men (2).
Intrinsic renal AKI is due to a pathologic process within the kidneys. It has a vast differential diagnosis. If there is no clear history of prerenal or postrenal AKI, intrinsic etiologies must be suspected. A thorough review of the patient’s past medical history, medications, and exposure to potential nephrotoxins is essential.
Risk factors for AKI could also be elicited on history taking. These include CKD, diabetes mellitus, older age, chronic liver disease, congestive heart failure, and renal artery stenosis (3).
Physical examination
In PTH-dependent hypercalcemia, PTH is inappropriately normal or high despite elevated calcium levels. The most common cause is primary hyperparathyroidism. 80% of these cases result from a single parathyroid adenoma. It can also be associated with hyperplasia of the parathyroid glands. Often, patients presenting with mild asymptomatic hypercalcemia will be found to have primary hyperparathyroidism (1).
Primary hyperparathyroidism can be distinguished from familial hypocalciuric hypercalcemia (FHH) by performing a 24-hour urine collection for calcium and creatinine. FHH is associated with a low calcium to creatinine clearance ratio (<0.01) whereas primary hyperparathyroidism would lead to a high ratio (>0.02). For practical purposes, urinary calcium to creatinine ratio or calcium concentration in a spot urine sample is often used for the initial evaluation of calciuria. If clinically indicated, calciuria can be confirmed with a 24-hour urine collection. FHH is an autosomal dominant condition caused by a calcium-sensing receptor gene mutation. It is important to distinguish between FHH and primary hyperparathyroidism as the management differs significantly. For example, parathyroidectomy is not appropriate for FHH (5). However, FHH is rare and usually benign. Hence, when faced with PTH-dependent hypercalcemia in clinical practice, physicians will often focus on ordering imaging studies of the parathyroid to assess for adenoma rather than the 24-hour urine collection.
Moreover, primary hyperparathyroidism may be a presentation of multiple endocrine neoplasia type 1 (MEN 1) syndrome, where parathyroid hyperplasia or adenoma occurs with pituitary and pancreatic islet tumors. It is also associated with MEN 2A syndrome, which is characterized by medullary thyroid carcinoma, pheochromocytoma, and parathyroid hyperplasia or adenoma. Hence, it is important to inquire about these associated conditions in such patients as well as perform a thorough family history. As these syndromes are hereditary, genetic testing is usually performed if there is a high clinical suspicion (5).
Other causes of PTH-dependent hypercalcemia include tertiary hyperparathyroidism. It occurs in patients with end-stage renal disease resulting in prolonged secondary hyperparathyroidism, high phosphate, and low vitamin D. Over time, this leads to autonomous PTH secretion unresponsive to plasma calcium levels. The drug lithium can also cause PTH-dependent hypercalcemia, which may be reversed if the drug is discontinued (3).
Initial laboratory investigations
Blood investigations: A complete blood count and full metabolic profile are ordered in the evaluation of AKI. The serum creatinine is important for the diagnosis of AKI and for monitoring its evolution (4). Some causes of AKI are associated with a characteristic timeline in terms of changes in serum creatinine. For instance, contrast nephropathy usually results in a rise of creatinine within 24-48h, peaks within 3-5 days, and resolves within a week. Moreover, hyperkalemia, hyperphosphatemia, and metabolic acidosis are possible complications of AKI (2).
A complete blood count is also useful in finding the etiology of the AKI. For instance, in a patient with suspected sepsis, an elevation in white blood cells could be present (2).
Urine investigations: Urinary tests are especially useful when trying to distinguish between prerenal AKI and acute tubular necrosis (ATN). In prerenal AKI, the tubular function is preserved and the kidneys increase sodium reabsorption and urinary concentration in response to decreased renal perfusion. However, this function is lost in ATN (5). The findings of both conditions are shown in Table 1.
| Table 1: Findings on urinary tests for prerenal acute kidney injury and acute tubular necrosis. | Prerenal | Acute tubular necrosis | |
| Urine sodium | <20 mmol/L | >40 mmol/L | |
| Fractional excretion of sodium | <1 | >2 | |
| Urine osmolality | >500 mOsm/kg | ~300 mOsm/kg | |
| Urine microscopy | Normal or hyaline casts | Renal tubular cell and granular casts (muddy brown) | |
Adapted from reference 5.
Urinalysis is part of the initial workup for AKI. It provides information regarding the concentration of the urine. It also detects proteinuria, white blood cells, and red blood cells in the urine. However, urinalysis only detects albumin. Therefore, assessing for the presence of other types of protein requires further testing (2).
Urine electrolytes and osmolality are also often obtained in the evaluation of AKI. A fractional excretion of sodium is calculated with the formula (100 x urinary sodium x serum creatinine) / (serum sodium x urinary creatinine). The units for urinary and serum creatinine are μmol/L while the units for the other measurements are mmol/L. It is important to note that for patients on diuretics, these values are less reliable (4).
Urine microscopy is particularly useful in the evaluation of AKI to assess for the presence of casts. Prerenal AKI is usually associated with an unremarkable urine microscopy although it occasionally presents with hyaline casts. Urine microscopy in postrenal AKI is usually unremarkable. Urine microscopy is especially helpful when assessing for intrinsic AKI. In ATN, tubular epithelial cell casts and granular (muddy brown) casts are seen. White blood cell casts are suggestive of acute interstitial nephritis. Red blood cell casts are seen in glomerulonephritis or vasculitic conditions. Most vascular causes of AKI other than vasculitis present with a normal urine microscopy (2).
Imaging: The use of a bladder scan to assess for the postvoid residual is a simple test for postrenal AKI. If the postvoid residual is greater than 200 mL, a below bladder obstruction should be suspected (4).
A renal ultrasound is also often ordered when evaluating for AKI. It is particularly helpful to rule out obstruction as the ultrasound could show hydronephrosis. Imaging studies such as computed tomography can also be used to visualize kidney stones or a neoplasm if they are suspected as the cause of the obstruction (4). Moreover, imaging may help in differentiating AKI and progression of CKD in patients whose baseline creatinine is unclear (3). In CKD, the kidneys usually appear smaller whereas the kidneys are of normal size in a patient with AKI without CKD. However, since CKD is most commonly caused by diabetic nephropathy, kidney sizes of CKD patients could also be normal (3).
Genetic testing: Usually, the above investigations provide a clear etiology for the AKI. However, genetic testing is occasionally used to assess for etiologies of AKI. For instance, atypical hemolytic uremic syndrome is commonly associated with genetic defects in the complement pathway and may lead to AKI. Hence, genetic testing in AKI could affect treatment decisions (3).
Beyond Initial Approach
Etiologies of AKI
Various etiologies of the prerenal, intrinsic, and postrenal AKI are presented in Table 2. Intrinsic causes of AKI are numerous and are broadly categorized as tubular, interstitial, glomerular, and vascular. A brief description of four common etiologies in each category will be provided below.
| Table 2: Etiologies of prerenal, intrinsic, and postrenal acute kidney injury. | Prerenal acute kidney injury | ||
| Intravascular volume depletion | Vomiting, diarrhea, poor oral intake, hemorrhage, diuretic overuse | ||
| Systemic vasodilation | Sepsis, anaphylaxis, cirrhosis | ||
| Intrarenal vasoconstriction/dilation | Congestive heart failure, cirrhosis, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers (dilation of efferent arteriole resulting in lower intraglomerular pressure), nonsteroidal anti-inflammatory drugs (constriction of afferent arteriole) | ||
| Intrinsic acute kidney injury | |||
| Glomerular | Post-infectious glomerulonephritis, anti-glomerular basement membrane disease, membranoproliferative glomerulonephritis, lupus nephritis, IgA glomerulonephritis, vasculitis | ||
| Interstitial | Acute interstitial nephritis | ||
| Tubular | Acute tubular necrosis | ||
| Vascular | Vascular, malignant hypertension, renal atherosclerotic emboli, hemolytic uremic syndrome, thrombotic thrombocytopenic purpura, scleroderma renal crisis, renal vein thrombosis | ||
| Postrenal acute kidney injury | |||
| Extrarenal obstruction | Benign prostatic hyperplasia, blocked catheter, malignancy, retroperitoneal fibrosis | ||
| Intrarenal obstruction | Nephrolithiasis, blood clots, malignancy | ||
Adapted from references 1 and 4.
Acute tubular necrosis (ATN): The most common cause of intrinsic AKI in hospitalized patients is ATN. The etiology is either ischemic from prolonged poor renal perfusion or nephrotoxic. Compared to prerenal AKI, the ischemic injury has resulted in tubular injury and the AKI does not improve with restoration of blood flow to the kidneys (4). Nephrotoxins are either endogenous or exogenous. For example, rhabdomyolysis and hemolysis both result in endogenous nephrotoxin-associated AKI, in part due to the direct tubular toxicity of myoglobin and hemoglobin respectively. In multiple myeloma, free light chains can also cause direct tubular toxicity (3). Exogenous nephrotoxins include contrast agents used in CT imaging and medications. Antimicrobial agents (e.g., vancomycin, amphotericin B, and acyclovir) and chemotherapy agents (e.g., cisplatin, carboplatin) are common culprits (2).
Acute interstitial nephritis: Acute interstitial nephritis is most commonly a result of medications such as antimicrobial agents, analgesics, proton pump inhibitors, anticonvulsants, and diuretics. However, it could also be associated with infections and systemic diseases, mainly rheumatologic (6). Patients present with fever, arthralgias, and a rash (2).
Glomerulonephritis: Glomerulonephritis (GN) encompasses diseases involving the glomerular podocytes, mesangial, and endothelial cells. They commonly present with red blood cell casts on urine microscopy (2). The laboratory investigations can suggest one particular cause of GN. For instance, elevated antineutrophil cytoplasmic antibody (ANCA) is associated with ANCA vasculitis. In another example, anti-glomerular basement membrane (anti-GBM) antibody is suggestive of anti-GBM disease. Also, low complement levels are seen in lupus nephritis, membranoproliferative GN, and postinfectious GN. Lastly, elevated antistreptolysin O titer is usually indicative of poststreptococcal GN. A kidney biopsy is often done if GN is suspected (4).
Hemolytic uremic syndrome: This condition usually follows a recent diarrheal episode and presents with the triad of AKI, thrombocytopenia, and microangiopathic hemolytic anemia (7). It is often due to the Shiga toxin released by bacteria such as \emph{Escherichia coli}. Clues in laboratory investigations include anemia, thrombocytopenia, elevation in LDH, and presence of schistocytes on blood smear (2).
Management of AKI
General principles: Management of AKI is directed at reversing the underlying cause. Moreover, supportive care is provided concerning fluid, electrolyte, and acid-base balance. It is also important to review the patient’s medications to discontinue nephrotoxic agents. Some medications’ dosing needs to be adjusted depending on the level of kidney function of the patient (3).
Correcting the underlying etiology: Prerenal AKI and ATN are often due to hypovolemia. Hence, the management includes the use of intravenous fluids. Isotonic fluids such as normal saline and Ringer’s lactate are usually chosen. Aggressive fluid resuscitation is also central to the treatment of AKI as a result of sepsis and anaphylaxis. Moreover, vasopressors are sometimes indicated to help maintain adequate perfusion. If AKI is secondary to congestive heart failure, cardiac function should be optimized (3).
The treatment of postrenal AKI depends on the site of the obstruction. As the most common etiology is benign prostatic hyperplasia, management of this condition with alpha blockers and 5-alpha reductase inhibitors improves the AKI. Some patients require a catheter to relieve the obstruction. The involvement of urology is usually encouraged in managing patients with postrenal AKI (3).
The management of intrinsic AKI is entirely dependent on the etiology. This is usually complex and above the scope of what a medical student is expected to know.
Supportive care: AKI can be complicated by various metabolic abnormalities. Metabolic acidosis is corrected with oral or intravenous infusion of sodium bicarbonate. Hyperkalemia also often occurs in patients with AKI. If there is presence of characteristic electrocardiogram changes, calcium gluconate must be administered immediately to stabilize cardiomyocyte membranes. Moreover, agents to shift potassium intracellularly (e.g., insulin, beta-agonists) and agents to increase elimination of potassium such as ion exchange resins may be used. Lastly, fluid overload is corrected with the use of diuretics (3).
Indications for initiation of hemodialysis: Some patients with AKI will require renal replacement therapy such as hemodialysis. The indications to initiate renal replacement therapy are metabolic acidosis, hyperkalemia, and volume overload refractory to medical management. Moreover, evidence of uremic pericarditis or encephalopathy is also an indication to start renal replacement therapy (4).
References
- Makris K, Spanou L. Acute Kidney Injury: Definition, Pathophysiology and Clinical Phenotypes. Clin Biochem Rev. 2016;37(2):85-98.
- Jameson JL, Kasper DL, Longo DL, Fauci AS, Hauser SL, Loscalzo J. Harrison's principles of internal medicine. 20th edition. ed. New York: McGraw-Hill Education; 2018.
- Gilbert SJ, Weiner DE, Bomback AS, Perazella MA, Tonelli M, National Kidney F. National Kidney Foundation's primer on kidney diseases. Philadelphia, PA [New York City, NY]: Elsevier; National Kidney Foundation; 2017.
- Rahman M, Shad F, Smith MC. Acute kidney injury: a guide to diagnosis and management. Am Fam Physician. 2012;86(7):631-9.
- Lerma EV, Sparks MA, Topf JM. Nephrology secrets. Philadelphia, PA: Elsevier; 2019.
- Kodner CM, Kudrimoti A. Diagnosis and management of acute interstitial nephritis. Am Fam Physician. 2003;67(12):2527-34.
- Canpolat N. Hemolytic uremic syndrome. Turk Pediatri Ars. 2015;50(2):73-82.
- Mathew AJ, George J. Acute kidney injury in the tropics. Ann Saudi Med. 2011;31(5):451-6.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.