Approach to
Strabismus
Arjan S Dhoot1 and
Michael J Wan2
Published online: March 4, 2022
1Faculty of Medicine, University of Toronto
2University of Toronto, Department of Ophthalmology and Vision Sciences; Hospital for Sick Children, Department of Ophthalmology and Vision Sciences
Corresponding Author: Arjan S Dhoot, email: arjan.dhoot@mail.utoronto.ca
DOI: 10.26443/mjm.v20i2.908
Abstract
Strabismus is characterized by a misalignment of the eyes commonly referred to as crossed eyes. A thorough physical examination and review of family history should be performed by clinicians when strabismus is suspected. The Hirschberg corneal reflex test, cover test, cover-uncover test, and alternate prism cover tests are commonly used to identify and diagnose strabismus. Strabismus requires a referral to an ophthalmologist. Treatment of strabismus may involve eye patches, cycloplegic drops, prescription glasses, and surgery. Strabismus can result in vision loss due to amblyopia, double vision, psychosocial concerns, and/or impaired depth perception.
Tags: Strabismus, Esotropia, Cover test, Cover-uncover test, Corneal light reflex, Ophthalmology
Case/Question
A 6-month-old girl is seen for her well-baby visit and is noted to have a "lazy" left eye. She has a normal birth history and there is no family history of ocular concerns. She meets all of her developmental milestones and is feeding well. Her parents say that her eyes have been like this since birth. On physical exam, the clinician noted that the left eye appears to be turned inwards. The Hirschberg corneal light reflex is notable for mild deflection of the light on the left eye temporal to the pupil. She is able to track toys and other objects well. Pupils are round, equal, and reactive to light and there is a normal red reflex in both eyes. No relative afferent pupillary defect is present. When the right eye is covered, the left eye moves outward to fixate. When the right eye is uncovered, the left eye turns in again. When the left eye is covered, the right eye is straight and fixating normally. When the left eye is uncovered, the right eye remains straight, but the left eye remains inwardly deviated. After dilating the pupils with eye drops, the clinician measures refractive errors on the right and left eye of +0.50 and +1.00, respectively. Physical examination is otherwise unremarkable.
What is the next best step?
- Patch the right eye
- MRI of the brain and orbits
- Patch the left eye
- Strabismus surgery to straighten the eyes
- Prescribe glasses for refractive error
Answer
A. Strabismus can result in vision loss due to amblyopia. To allow for correction, the strong eye should be covered with a patch to allow the amblyopic “lazy” eye to return to normal function. It is also important to check for refractive error, which may help to treat both strabismus and amblyopia in certain circumstances. Strabismus surgery in this case may be indicated, but the most important first step is to start treating the amblyopia.
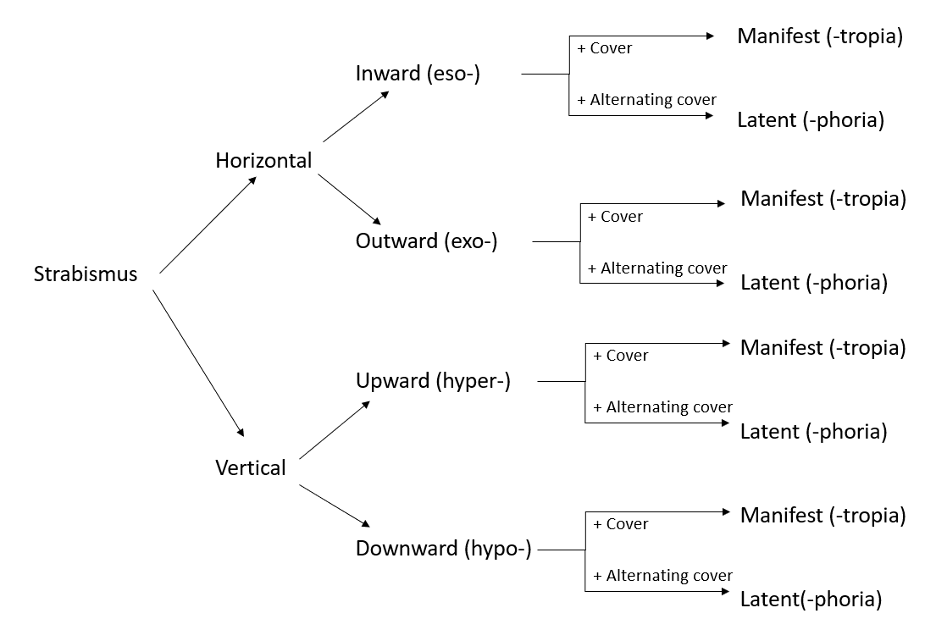
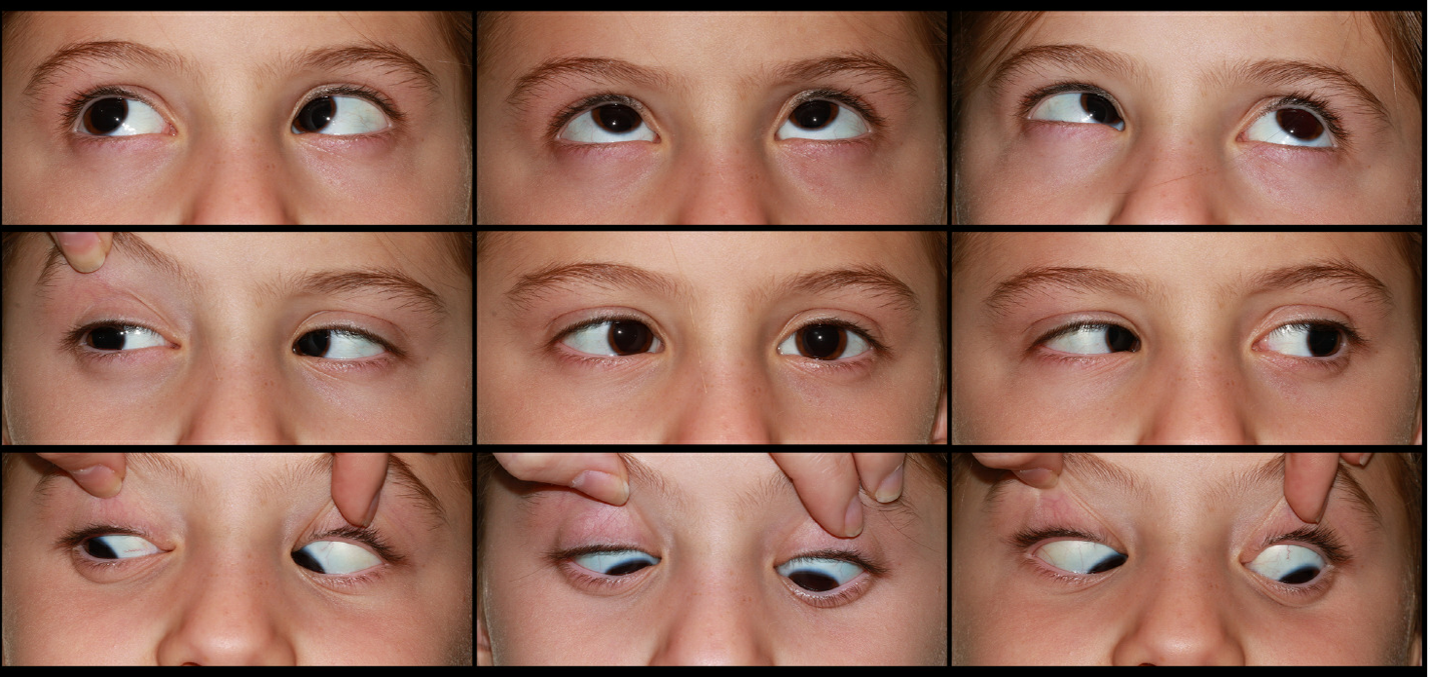
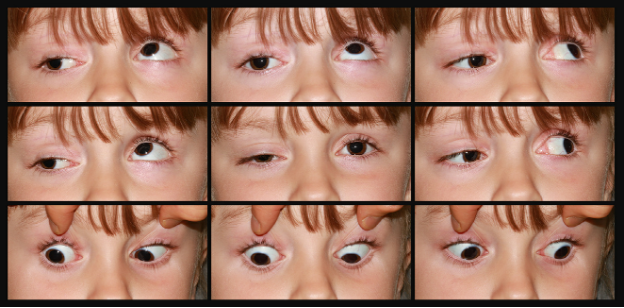
Initial approach
Strabismus is defined as an ocular misalignment. (1) It is classified by the alignment of the eyes relative to each other and can be either horizontal or vertical. The two forms of strabismus are tropia (manifest deviation, or present when an individual views a target with both eyes open) and phoria (latent deviation, or present only when one eye is occluded). Manifest deviations can be diagnosed with the cover test and latent deviations can be diagnosed with a cover/uncover or alternate prism cover test. This approach is summarized in Figure 1. Figures 2 and 3 demonstrate an exotropia and hypertropia, respectively.


Deviations can be further classified as constant or intermittent. A constant deviation is always present while an intermittent deviation is only present in specific situations, such as when the patient is fatigued or ill. In addition, deviations can be classified as comitant and incomitant. Comitant deviations are the same degree in all positions of gaze while incomitant deviations are more pronounced in certain positions of gaze. Comitant deviations are more common and usually benign, while incomitant deviations are uncommon and frequently a sign of serious underlying pathology. Comitant and incomitant deviations are demonstrated in Figures 4 and 5, respectively.
To summarize with an example, a patient presents with a horizontal deviation with their left eye always turning inward and not changing with the position of gaze. On examination, they have a positive cover/uncover test. This would be classified as a left constant, comitant, esotropia. Of note, esotropia is the most common form of strabismus. (2)
Beyond the Initial Approach
To better understand strabismus, we present the relevant anatomy, etiology, important components of history-taking, physical examination, special tests, and available treatments.
Strabismus is the result of ocular misalignment, so it is important to be familiar with the function of the 6 extraocular muscles that control eye movement and their innervation. The extraocular muscles are innervated by three cranial nerves (CN). CN VI (abducens nerve) controls the lateral rectus muscle which moves the eye laterally. A CN VI palsy typically presents with an incomitant esotropia and should raise suspicion for elevated intracranial pressure. CN IV (trochlear nerve) controls the superior oblique muscle which internally rotates the move and moves it downward when the eye is looking inward. A CN IV palsy presents with a head tilt away from the side of the palsy. CN III (oculomotor nerve) controls the remaining muscles of eye movement (superior rectus, inferior rectus, medial rectus, and inferior oblique). In addition, CN III is involved in elevation of the eyelid via innervation of the levator palpebrae superioris muscle and constriction of the pupil via parasympathetic innervation of the sphincter pupillae. CN III palsy presents as a “down and out” eye with a fixed, dilated pupil, and ptosis. (3) Detailed diagrams regarding the anatomy of the orbit, extra-ocular muscles, and cranial nerves are available in orbital anatomy textbooks. (4)
Strabismus is most frequently diagnosed in children and can lead to amblyopia, which is permanent reduced visual acuity in a one eye due to abnormal visual development early in life. Strabismus in adults usually causes diplopia. Normally, the eyes work together to produce similar images that are combined by the visual cortex to allow for depth perception and three-dimensional vision. In children with strabismus, the images from the eyes are too disparate for the brain to combine into a single image. Over time, the brain will suppress (i.e., learns to ignore) one of the eyes which may lead to amblyopia. This will potentially cause a permanent loss of vision in the suppressed eye and a failure of binocular vision to develop normally. Adults rarely develop amblyopia because the visual cortex has already developed. An ocular misalignment can also have a significant impact on psychological development which can lead to deficiencies later in life in terms of social development and maturity. (5) Children with untreated strabismus are more likely to live in areas of lower socioeconomic status and have a low quality of life. (6) Increased screening and education has resulted in a lower global prevalence of amblyopia secondary to strabismus, yet it remains a significant cause of vision loss in children, particularly in immigrant and lower socioeconomic communities due to reduced access to healthcare. (7)
A specific cause of strabismus is not determined in many cases. Strabismus is thought to be multifactorial in nature with contributions from genetic and environmental influences. Both congenital and acquired forms of strabismus exist and it is important to differentiate between the two as an acquired strabismus is a red flag for conditions such as Down Syndrome, cerebral palsy, hydrocephalus, muscular dystrophy, or a cranial mass. (8) There are many risk factors for the development of strabismus. The strongest risk factors for congenital strabismus are anisometropia (Odds Ratio (OR): 7.79), maternal inheritance (OR: 6.42), and critical retinopathy of prematurity (OR: 5.89). (9) Other contributing factors include low birth weight, prematurity, and maternal smoking during pregnancy. (9) The prevalence of congenital strabismus in the general population is estimated to range from roughly 1 to 5%. (10) Acquired strabismus is more common in adults and can result from trauma, surgical procedures, cranial nerve palsies, thyroid dysfunction, and other neurological processes, such as a stroke. The incidence rate of acquired strabismus is roughly 54 cases per 100,000 individuals, or roughly 0.05%. (11)
For primary care physicians, it is important to conduct a comprehensive history and organized physical examination for patients with suspected strabismus. The history must be broad and include risk factors for the development of strabismus. Clinicians should determine if there are any co-morbid conditions, including neuromuscular conditions that can affect eye development and how the brain interprets visual information. A thorough developmental and birth history should be taken as premature/low birth weight is a risk factor for strabismus. It is important for clinicians to note when the strabismus started to determine if it is a congenital or acquired strabismus. It is also essential to characterize whether the strabismus has any triggers and if it is constant or intermittent. As well, the presence of double vision can be an critical clue regarding the presence of strabismus. It should also be clarified whether the child has any other medical or ocular problems. For example, a child who is squinting to focus may have significant refractive error, which is a risk factor and potential cause of strabismus. Lastly, a family history of strabismus should also be explored as this is a major risk factor for developing the condition.
An organized approach should be taken for the physical examination. Any abnormal head posturing including head tilts, turns, and rotations should be noted, as these may indicate accommodative actions taken by the patient to prevent diplopia. Inspection of the eyes should start by observing for position and alignment. Furthermore, the eyelids should be examined for any asymmetry, lid edema, discolorations, or signs of trauma. First, the extraocular movements should be assessed with the six cardinal positions of gaze. During this examination, careful attention should be paid to any restrictions in extraocular motility or any misalignment of the eyes in any position of gaze. Next, visual acuity and colour vision should be assessed with the patient wearing prescription glasses if they have them using age-appropriate options for visual acuity assessment. Lastly, confrontational visual fields and pupils should be assessed for size, symmetry, and reactivity to light.
During the physical examination, in addition to the aforementioned tests, the following specialized tests specifically for strabismus should be employed. The Hirschberg corneal light reflex test assesses for ocular alignment by observing the location of the corneal light reflex relative to the centre of the pupil (Figure 2). To administer this test, the clinician should direct a pen light at the patient and ask them to look directly at it. Individuals with strabismus will have a deviation of the light reflex. In patients with esotropia, exotropia, hypertropia, or hypotropia the cornea light reflex will be displaced temporally, nasally, inferiorly, or superiorly, respectively. The cover test and cover-uncover test should be employed to determine the presence of a manifest deviation or latent deviation, respectively. To perform the cover test, the patient should fixate ahead and cover one of their eyes. A positive cover test occurs when the uncovered eye moves when the contralateral eye is covered. The cover-uncover can be performed by asking the patient to fixate and have them cover the eye. Next, the cover is quickly removed and the examiner notes if there are any movement in the previously covered eye. A positive cover-uncover test occurs when the covered eye moves after removal of the eye cover. Videos of the cover test and the cover-uncover test are available on the American Academy of Ophthalmology website.(12) Lastly, the red reflex should be assessed with direct ophthalmoscopy. Absence of a red reflex can indicate conditions such as retinoblastoma, which should be referred urgently to a pediatric ophthalmologist to perform a dilated fundus examination.
The overall goal of treatment for patients with amblyopia is to improve the vision in the affected eye as much as possible. The primary treatment is with patching of the fellow (dominant) eye. Part-time patching of the fellow eye encourages usage of the amblyopic eye to strengthen and improve vision. Another option includes the usage of dilute cycloplegic drops in the fellow eye, typically atropine. Atropine temporarily impairs accommodation and blurs vision in the stronger eye, particularly at near, forcing the child to use the amblyopic eye to see.
The primary goal of strabismus treatment is to realign the eyes, which can be achieved with different treatments depending on the underlying pathology. In certain types of strabismus, prescription glasses can correct refractive errors and treat it. Strabismus surgery is often needed for conditions not amenable to refractive correction. Certain types of strabismus are signs of serious underlying pathology and require a workup prior to correction of the misalignment. For instance, an acute-onset CN VI palsy may indicate intracranial disease and needs an urgent workup.
In conclusion, strabismus is an ocular misalignment that can cause vision loss due to amblyopia. It is important to be aware of how to test for strabismus and, in particular, how to identify types of strabismus that are signs of serious underlying pathology. Treatment of amblyopia typically requires covering or blurring the dominant eye, while treatment of strabismus is usually achieved with prescription glasses or surgery.
References
- Gunton KB, Wasserman BN, DeBenedictis C. Strabismus. Primary Care - Clinics in Office Practice. 2015.
- Faisal Fahim M. Prevalence of Strabismus and its type in Pediatric age group 6-15 years in a tertiary eye care hospital, Karachi. Biometrics Biostat Int J. 2019;
- Sonne J, Lopez-Ojeda W. Neuroanatomy, Cranial Nerve. StatPearls. 2019.
- Dutton J. Atlas of Clinical and Surgical Orbital Anatomy. 2nd ed. Elsevier; 2011.
- Chia A, Dirani M, Chan YH, Gazzard G, Au Eong KG, Selvaraj P, et al. Prevalence of amblyopia and strabismus in young singaporean chinese children. Investig Ophthalmol Vis Sci. 2010;
- Durnian JM, Owen ME, Baddon AC, Noonan CP, Marsh IB. The psychosocial effects of strabismus: Effect of patient demographics on the AS-20 score. J AAPOS. 2010;
- Shapira Y, Machluf Y, Mimouni M, Chaiter Y, Mezer E. Amblyopia and strabismus: Trends in prevalence and risk factors among young adults in Israel. Br J Ophthalmol. 2018;
- Merrill KS, Lee MS, McClelland CM. Red Flags in the Assessment of Adult Ophthalmoplegia. J Binocul Vis Ocul Motil. 2018;
- Maconachie GDE, Gottlob I, McLean RJ. Risk Factors and Genetics in Common Comitant Strabismus: A Systematic Review of the Literature. JAMA Ophthalmol. 2013;
- Han KE, Baek SH, Kim SH, Lim KH. Prevalence and risk factors of strabismus in children and adolescents in South Korea: Korea national health and nutrition examination survey, 2008 - 2011. PLoS ONE. 2018.
- Martinez-Thompson JM, Diehl NN, Holmes JM, Mohney BG. Incidence, types, and lifetime risk of adult-onset strabismus. Ophthalmology. 2014;
- American Academy of Ophthalmology. Basic and Clinical Science Course: Section 06: Pediatric Ophthalmology and Strabismus [Internet]. [cited 2022 Jan 9]. Available from: http://aao-resources-enformehosting.s3.amazonaws.com/resources/

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.