Case Report
Distal Radial Artery Ligation for Dialysis Access Steal Syndrome
David Fung1, Yaasin Abdulrehman2
Published online: September 22, 2021
1University of Alberta
2Department of Surgery, University of Alberta
Corresponding Author: David Fung, email fung1@ualberta.ca
DOI: 10.26443/mjm.v20i2.898
Ethics Statement
Patient verbal and written consent was obtained for this case report. Patient demographic details have been modified where applicable to maintain patient confidentiality and only clinically relevant details are used. Ethics Committee approval was not required for this case report.
Abstract
Renal replacement therapy is the definitive treatment for end-stage renal disease apart from transplant. Steal syndrome, which can lead to distal limb ischemia, is a rare but serious complication in patients who undergo hemodialysis with an arteriovenous fistula. We present a case of a 48-year-old female with limited options for dialysis access who presented with symptoms of steal syndrome. Given the need to keep her current fistula, we opted to treat her with distal radial artery ligation. This case report summarizes the various surgical techniques available for treating dialysis access-associated steal syndrome and why distal radial artery ligation should be considered a viable management strategy, especially in the context of our patient.
Tags: Renal replacement, Dialysis, Vascular surgery, Fistula, Steal syndrome, AV fistula, Ischemia
Introduction
For patients with end-stage renal disease (ESRD), renal replacement therapy is the only available treatment option unless a transplant is indicated. Patients have the option of undergoing hemodialysis or peritoneal dialysis. For hemodialysis, access can be achieved through surgical creation of an arteriovenous (AV) graft, insertion of a hemodialysis catheter, or by creation of an arteriovenous fistula (AVF). Radiocephalic fistulas are the most frequently created access fistulas. (1)
On average, the maturation rate of radiocephalic fistula is about 75%. (2) For those that do mature, we then consider the development of complications with the fistula. Complications, although rare, can be serious. They include bleeding, infection, neuropathy leading to carpal tunnel syndrome, hand venous hypertension, radial artery segmental occlusion, aneurysmal dilation of the axillary and brachial arteries, and thrombosis. (1) A steal phenomenon may also occur causing retrograde flow in the radial artery distal to the anastomosis. Physiologic steal occurs due to the flow shunt and can be seen in about 70% of all radiocephalic fistulas. (3) However, ischemic steal phenomena that contribute to distal hand ischemia and other complications are known as dialysis access-associated steal syndrome (DASS). DASS is a rare complication and occurs in 1-2% of all radiocephalic fistulae. (3)
We present a case of DASS in a 48-year-old female with a left forearm radiocephalic fistula successfully treated with distal radial artery ligation (DRAL).
Case Description
Patient is a 48-year-old female with a history of ESRD secondary to IgA nephropathy, failed kidney transplant, numerous failed peritoneal dialysis catheters, and is currently hemodialysis dependent via a left forearm radiocephalic fistula. She presents to a dialysis access clinic with symptoms of hand weakness along with pain, paresthesia, and discolouration. Pain was localized to the hand with no specific distribution to the fingers, which had been progressively worsening over the course of 5-6 months. Physical exam revealed an easily palpable thrill in her fistula and palpable ulnar and radial pulses. We performed a bedside ultrasound to assess the patency and flow in the arteries and veins. The patient was then assessed with a formal ultrasound and fistulogram.
A formal ultrasound was performed to assess the direction of flow in the distal radial and ulnar arteries, and in the proximal and distal radiocephalic anastomosis. There was antegrade flow in the ulnar artery which exclusively supplies the palmar arch. Proximal to the level of the radial cephalic fistula, there was normal antegrade flow in the proximal radial artery (Fig. 1A). However, distal to the level of the fistula, there was abnormal retrograde flow in the distal radial artery consistent with an arterial steal phenomenon (Fig. 1B)
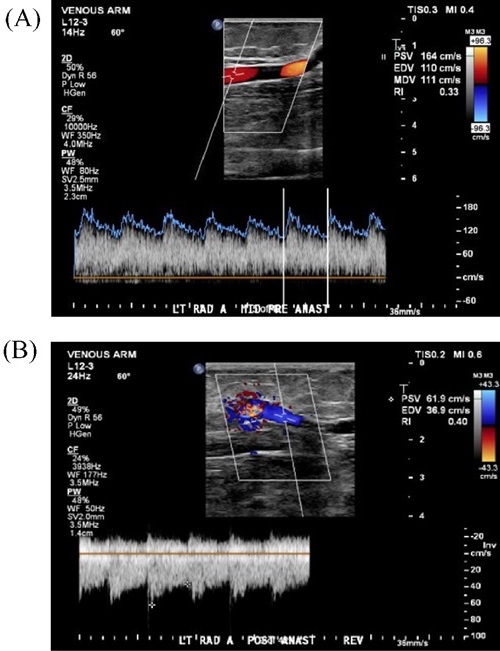
(A) Doppler of the radial artery proximal to the level of the anastomosis demonstrating anterograde flow.
(B) Doppler of the radial artery distal to the level of the anastomosis demonstrating retrograde flow as evidenced by reversed flow velocities. The anastomosis is demonstrated in the upper left portion of the Doppler window where there is speckling of the flow diagram.
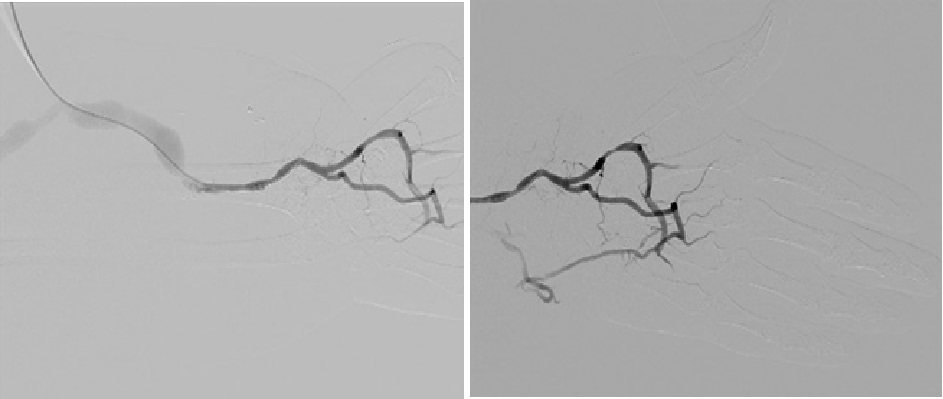
A fistulogram demonstrated wide patency of the radial artery, radiocephalic anastomosis, and forearm cephalic vein. Retrograde flow in the left distal radial artery also suggests an arterial steal phenomenon. No flow-limiting stenosis was seen in the superficial or deep palmar arch (Fig. 2).
Given that the patient had a distal radiocephalic fistula, DASS was at the top of our differential diagnosis. Other conditions that cause neuropathy were considered on our differential. Carpal tunnel syndrome was suspected; however, the patient did not notice temporal changes to her symptoms, nor did she reveal any signs on physical exam. Vasculitis that causes nerve ischemia or diabetic neuropathy were both considered as well, but the patient did not have a past medical history suggestive of these. Lastly, abscess or hematoma related neuropathy was also part of the differential diagnosis.
Treatment
Ultrasound was used to mark the radial artery preoperatively. We made a small 2-cm incision, dissected and identified the radial artery, and encircled it with a vessel loop. We performed Doppler analysis of the radial artery with temporary ligation of the distal radial artery and the flow became triphasic, which is normal for peripheral arteries. Satisfied with the Doppler, the distal radial artery was formally ligated. Successful ligation of the artery resulted in a good, sustained flow into the ulnar artery and palmar arches as witnessed by the Doppler. The AVF maintained a very strong thrill. We were able to successfully ligate the radial artery distal to the AVF and maintain good forward flow into the hand via the ulnar artery without compromising flow into the fistula.
Outcome and Follow-up
The patient was stable out of the operation and recovered without complications. Subjectively, the patient experienced symptomatic relief immediately after the recovery phase. The patient was doing well upon discharge with no compromise in AVF function. At her 9-month follow-up, she was self-cannulating her left forearm fistula successfully using two-needle rope ladder cannulation and running at our institution’s maximum dialysis speed. Point-of-care ultrasound demonstrated transonic flows at 1700-1780 mL/min, suggesting normal flow.
Discussion
There are many strategies to approach DASS: distal radial artery embolization (DRAL), proximal radial artery ligation (PRAL) for reduction of flow, revision using distal inflow (RUDI), distal revascularization and interval ligation (DRIL), proximalization of the arterial inflow (PAI), fistula banding, and ligation of the fistula. (4) The most common intervention is ligation of the AVF and creation of a new fistula in another location.
With our patient, preservation of fistula access was important due to her history of repeated failures of intraperitoneal catheters and thrombosis of central access lines, notwithstanding the fact that central lines are not permanent solutions for dialysis access. The main decision for this patient then was to either create a new fistula or to salvage the current fistula. Creation of a more proximal fistula in this patient was not ideal since DASS is more common for proximal fistulas. (3) Ligation of the current fistula and creating a new fistula in the other arm was not a preferred option as she is a young patient and we wanted to preserve future access sites. Therefore, effort was made to salvage her current fistula.
We can then approach the various treatment procedures in terms of the end goal of reducing flow across the fistula. With regards to actual intervention at the level of the fistula, banding decreases the diameter of the fistula, thus increasing resistance and decreasing flow. We can also think of altering the sources of flow that contribute to the steal phenomenon. These include PRAL, RUDI, DRIL and DRAL. PRAL, RUDI and DRIL are employed for more proximal AVFs such as brachiocephalic fistulas, which our patient did not have. Options for our case thus included fistula banding, PRAL, and DRAL. For our patient, fistula banding was not pursued since it has a higher re-intervention rate and a higher rate of access thrombosis. (4) PRAL was not selected since the surgeon was concerned that it may compromise flow to the fistula thus rendering it non-functional. It is estimated that one-third of radiocephalic fistula flow is supplied by the distal radial artery, so by preserving proximal flow, which conversely supplies two thirds of normal fistula flow, we may theoretically conserve flow through the fistula. (5) Although distal radial artery embolization is a newer technique, DRAL should still be considered given its ease and ability to assess flow intraoperatively. For the above reasons and surgeon experience, DRAL was chosen as the ideal approach for this patient.
Ultrasound is vital in our approach to our patient. Preoperative examination using colour doppler ultrasound can be used to predict the success of DRAL. (6) It is therefore beneficial to use point-of-care ultrasound in the initial assessment in the clinic to help guide therapy.
DRAL is an effective procedure and should be considered. A study of patients with DASS within a 5-year period from one centre demonstrated that procedures were mostly ligation (50%) or banding (38%). (4) However, our case demonstrates that DRAL is a viable and effective treatment for radiocephalic fistulas. Disruption of distal flow using DRAL has been shown to be very efficacious with small subpopulations in epidemiologic studies showing 100% symptom resolution with no vascular comorbidities. (4,7) In a study looking at 15 DASS patients where 5 of which underwent DRAL, all showed significant clinical improvement in clinical symptoms. Of the patients with DRAL, 3 of the 5 had complete resolution. The two patients with partial resolution had complications due to significant pre-existing comorbidities. Hence, DRAL is an efficacious technique in most DASS patients with radiocephalic fistulas.
Learning Points and Conclusion
Patient context will often guide one’s therapeutic decision making. In our case, our dialysis patient was experiencing DASS with a history of multiple failed access attempts using intraperitoneal dialysis. The patient’s young age also pushed us toward trying to salvage the current fistula as opposed to ligating the current fistula and creating a more proximal fistula. Given her age and dependency on fistula access, it was more advisable to maintain access options for the future.
Ultrasound and angiographic assessment are vital in determining the success of a DRAL procedure and should be a part of any work-up in deciding treatment for DASS. With our patient, DRAL is a successful treatment for DASS. Disruption of distal radial artery flow has been shown to be a successful strategy in relieving ischemic steal-related symptoms. (7) Given appropriate collateral flow from the ulnar into the palmar arch, DRAL should be considered in patients with radiocephalic fistula DASS.
References
- Mousa AY, Dearing, DD, Abu Rahma AF. Radiocephalic Fistula: Review and Update. Annals of Vascular Surgery. 2013;27(3):370-378. doi: 10.1016/j.avsg.2012.07.012.
- Chan C, Ochoa CJ, Katz SG. Prognostic Factors for Arteriovenous Fistula Maturation. Ann Vasc Surg. 2018;49:273-276. doi: 10.1016/j.avsg.2018.01.069.
- Zamani P, Kaufman J, Kinlay S. Ischemic steal syndrome following arm arteriovenous fistula for hemodialysis. Vascular Medicine. 2009;14(4):371-376. doi: 10.1177/1358863X09102293.
- Leake AE, Winger DG, Leers SA, Gupta N, Dillavou ED. Management and outcomes of dialysis access-associated steal syndrome. Journal of Vascular Surgery. 2015;61(3):754-76. doi: 10.1016/j.jvs.2014.10.038
- Bourquelot P, Gaudric J, Turmel-Rodrigues L, Franco G, Van Laere O, Raynaud A. Proximal radial artery ligation (PRAL) for reduction of flow in autogenous radial cephalic accesses for haemodialysis. Eur J Vasc Endovasc Surg. 2010 Jul;40(1):94-9. doi: 10.1016/j.ejvs.2010.02.007.
- Cordova E, Pettorini L, Scrivano J, Baldinelli M, Punzo G, Menè P, Pirozzi N. Preoperative duplex examination in patients with dialysis access-related hand ischemia: indication for distal radial artery ligation. J Vasc Access. 2015;16(3):255-257. doi: 10.5301/jva.5000341
- Miller GA, Khariton K, Kardos SV, Koh E, Goel N, Khariton A. Flow interruption of the distal radial artery: treatment for finger ischemia in a matured radiocephalic AVF. J Vasc Access. 2008;9(1):58-63. doi: 10.1177/112972980800900110

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.