Brief Report
The Effect of Perceived Weight Gain on Hormonal Contraception Choice for Women: A Review
Joni Roberts1
Published online: July 5, 2022
1California Polytechnic State University - San Luis Obispo, USA.
Corresponding Author: Joni Roberts, email: jrober81@calpoly.edu
DOI: 10.26443/mjm.v20i2.886
Abstract
Background: Hormonal contraception plays a pivotal role in protecting against unintended pregnancies and has been developed to provide options that best fit women's lifestyles. However, negative perceptions can alter women's attitudes and prohibit the use of hormonal contraception. This review aimed to collect information surrounding perceptions of side effects due to hormonal contraception, specifically, perceptions of weight gain, and their influence on women's contraceptive choice.
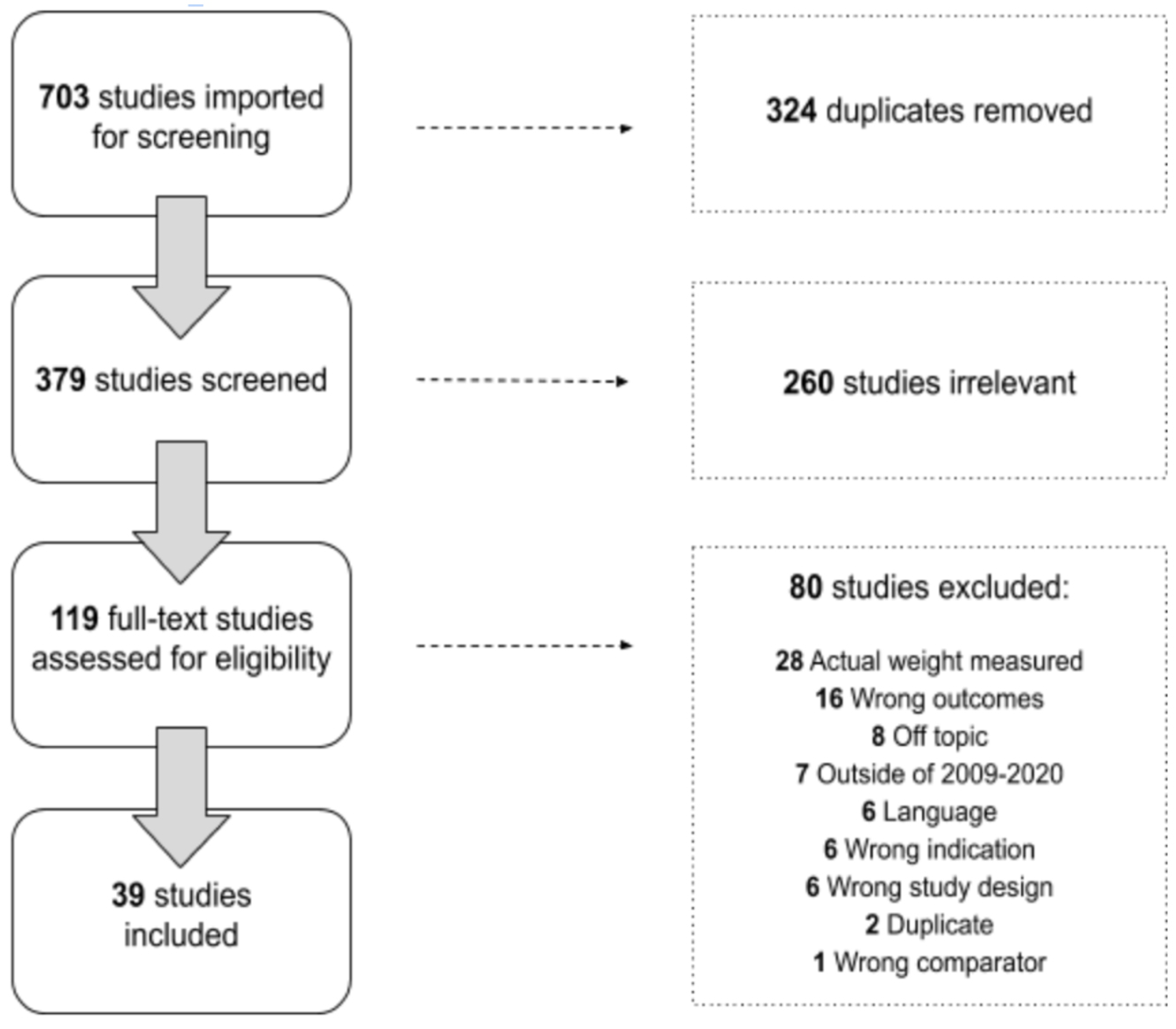
Methods: 703 articles were found through searching three electronic databases: EBSCO, PubMed, and Web of Science; in addition to Google Scholar. Articles were included if published between 2009-2020, could be translated to English, included any form of hormonal contraception, and reported perceived weight gain. A total of 39 articles met the inclusion criteria and were included in the review.
Results: Within those articles, there were six overarching themes: (1) negative perception of weight gain, (2) fear of weight gain, (3) contraception decision based on obesity concerns, (4) avoidance and discontinuation of the hormonal contraception due to concerns of weight gain, (5) limited contraceptive knowledge, and (6) lack of counseling. Women’s perceptions and attitudes of contraceptive methods were shaped by both belief and perceptions, i.e., women who believed weight gain a side effect of HC and/or had negative perceptions of contraceptive related weight gain influenced their overall perceptions and attitude of a contraceptive method.
Conclusions: Negative perceptions are derived from experience, misconception, and lack of knowledge; this leads to fear, avoidance, or discontinuation. Understanding women's perceived weight gain and perception towards contraceptives can help assess its effect on women's choice of contraception. This information can aid health care professionals in educating and discussing methods that would best fit women and improve hormonal contraception adherence.
Tags: Hormonal Contraception, Weight, Perception, Women
Background
Family planning methods, specifically hormonal contraception (HC), have become increasingly popular globally among individuals of reproductive age. Commonly used HC methods include oral contraceptive pills, vaginal rings, injectable contraceptives, transdermal contraceptive patches, and long-acting reversible contraceptives (LARCs): intrauterine devices (IUDs) and contraceptive implants. Women seek HC for their effects on pregnancy prevention, menstrual consistency, and acne control. Method effectiveness and longevity can vary, allowing users to choose the method that best fits their lifestyle.
While the effectiveness of HC methods can be appealing, their side effects can deter use and adherence. With more women reporting weight gain as a side effect, studies have tried to understand the role of HC methods on weight gain. Gallo and Lopez conducted a systematic review that found no evidence that pills or patches caused any weight change. (1) While there is a lack of scientific consensus on whether pills, patches, rings, and IUDs induce weight change, injectable HC has been shown to cause weight gain (mean weight gain of >2kg). (2) Women are more likely to use oral contraceptives (88%) than injectable contraceptives (23%). Therefore, women who use oral contraceptives as their HC method should not experience the side effect of weight gain. (3)
Since the 1960s, the percentage of US women who are overweight, obese, or severely obese has consistently been higher than that of males. (4) Furthermore, the proportion of women transitioning from normal to overweight and overweight to obese has increased annually since the 1960s. (4) As women perceive themselves at risk for obesity, fear of weight gain becomes more prominent. Women with obesity concerns may view weight gain from HC as detrimental. This can influence their perception (consciousness) and attitude (feeling/emotion), thus creating a barrier to contraceptive adherence regardless of BMI.
Many articles have studied actual weight gain caused by hormonal contraceptives, but few attended to the perceptions of weight change and how they affect the use of contraception. This literature review strived to examine the relationship between perceived weight gain from hormonal contraceptives and contraceptive decisions among women of reproductive age.
Method
Search Strategy
Data were retrieved from EBSCO, Google Scholar, PubMed, and Web of Science between January and February 2020. The initial search included studies related to hormonal contraception and perceived weight change in women. The final keywords included: discontinuation; weight perception; body weight; birth control; weight gain; hormonal contracept*; perceived weight; qualitative; side effects; body image; knowledge, attitudes, and behaviors. An emphasis was placed on searching perceived weight gain and qualitative data to find self-reported data rather than actual measurements of weight gain while using HC methods. The final search terms are outlined in Table 1.
| Table 1: Search terms | Data Bases | Search Terms | Exclusion Terms |
| Web of Science |
- BIOSIS Previews - Web of Science Core Collection - MEDLINE |
- Contracep* “side effect” AND weight AND qualitative - “Body weight” OR “body perce*” AND contracep* - Weight percept* OR perce* weight AND contracep* - Contracep* AND weight AND qualitative - Knowledge OR attitudes OR beliefs AND contracep* AND weight - “Body image” OR “body weight” AND contracep* - “Weight percep*” OR “weight gain” OR “body image” OR “percei* weight” AND contracep* |
- emergency OR –abort* OR –male OR –fert OR -” unintended pregnancy” |
| EBSCO | - CINHAL plus with full text - Academic Search Premier |
- Contracep* “side effect” AND weight AND qualitative - “Body weight” OR “body perce*” AND contracep* - Weight percept* OR perce* weight AND contracep* - Contracep* AND weight AND qualitative - Knowledge OR attitudes OR beliefs AND contracep* AND weight - “Body image” OR “body weight” AND contracep* - “Weight percep*” OR “weight gain” OR “body image” OR “percei* weight” AND contracep* |
- emergency OR –abort* OR –male OR –fert OR -” unintended pregnancy” |
| Google Scholar | - Contracep* AND “side effect” AND weight AND qualitative - Contracep* AND “body weight” OR “body perce*” - “Weight percept*” OR “perce* weight” AND contracep* - “Birth control” AND weight AND qualitative - Contracep* AND weight AND knowledge OR attitudes OR belief - “Body image” OR “body weight” AND contracep* - “Weight percep*” OR “weight gain” OR “body image” OR “percei* weight” AND contracep* |
- emergency OR –abort* OR –male OR –fert OR -” unintended pregnancy” | |
| PubMed | - Contracep* “side effect” AND weight AND qualitative - “Body weight” OR “body perce*” AND contracep* - Weight percept* OR perce* weight AND contracep* - Contracep* AND weight AND qualitative - Knowledge OR attitudes OR beliefs AND contracep* AND weight - “Body image” OR “body weight” AND contracep* - “Weight percep*” OR “weight gain” OR “body image” OR “percei* weight” AND contracep* |
- emergency OR –abort* OR –male OR –fert OR -” unintended pregnancy” | |
Inclusion and Exclusion Criteria
Articles were included if published between 2009-2020, written in any language, focused on any country, studied at least one hormonal contraceptive, and included self-reported or perceived weight gain due to HC methods. Articles were excluded if they discussed emergency contraceptives, abortions, male contraceptives, or actual reports of weight gain. Articles unable to be translated to English were also excluded. Actual weight gain was a quantitative measurement of weight change, i.e., body mass index (BMI), pre & post-weight measurements. Perceived weight gain was defined as the patient's self-reported, qualitative opinions about perceived weight changes while using HC methods.
Selection process
Covidence online software was used to manage the review process, as displayed in Figure 1 (Covidence systematic review software). The initial search resulted in 703 articles. After removing duplicates, 379 articles remained. Those 379 articles were then screened by title and abstracts by a team of five researchers. Two votes were required to include/exclude the articles, and the primary investigator resolved all conflicts. Through the abstract screening process, 119 articles proceeded to full-text screening, 80 of which were removed. A total of 39 articles were thus included in the review.
Results
Study Characteristics
Most articles discussed negative perceptions of weight gain from hormonal contraceptives (69%, N=39). Sixteen (41%, N=39) articles examined women of all reproductive ages, while another sixteen studied married women (39.0%, N=39), and seven focused on adolescents or college-aged women (17.0%, N=39). Studies varied in contraceptive method focus: multiple family planning methods including condoms, vasectomy, and hormonal contraceptives, hormonal contraceptives only, oral contraceptives, IUDs, injections, LARCs, ring, implants. (2, 3, 5, 8, 13) Thirty-six studies focused on perceived adverse effects regarding hormonal contraceptive side effects, while three studies examined the perception of both positive and negative effects. Weight gain as a side effect was identified in twenty-seven studies. The detailed characteristics of the studies are summarized in Table 3. In general, articles displayed six overarching themes: (1) negative perception of weight gain, (2) fear of weight gain, (3) contraception decision based on obesity concerns, (4) avoidance and discontinuation of the contraceptive method due to concerns of weight gain, (5) limited contraceptive knowledge, and (6) lack of counseling. The detailed characteristics of the studies and themes are summarized in Table 2.
| Table 2: Article characteristics. | Location | Contraceptive | Participant Characteristics | Findings | |||
| Agasti et al., 2017 | Orissa, India | Family planning methods (condom, OCP, IUD, vasectomy, etc.) | n=36
age=N/A Setting: tribal health center |
Questionnaires administered to healthcare workers found that they may have pre-existing biases against weight gain from contraceptives and could be influencing their clients’ biases during consultations. | |||
| Al-Mass et al., 2018 | Riyadh, Saudi Arabia | Oral contraceptive pill |
n=462
age=14-50 Setting: public shopping mall |
More married women perceived weight gain than unmarried women. Regular OC users perceived more weight gain than irregular OC users. The article also noticed the belief that OCs will cause weight gain. | |||
| Altaf et al., 2017 | Chicago, US | Birth control | n=23 (focus group), 1442 (survey)
age=N/A Setting: focus group discussions |
Survey was administered to college women to which 23/1442 were engaging in sexual behaviors without contraception due to fear of weight gain from contraceptives. Women with low body shame scores showed that negative body im age correlates to fear of weight gain from contraceptive. |
|||
| Bajwa et al., 2011 | Punjab, India | Condom, Oral contraceptive pill, IUD | n=1123
age=15-49 Setting: Rural Health Training Center |
A survey done in India determined that pills were perceived to cause weight gain as shown by the 38% who were not using OCP due to fear of weight gain. | |||
| Bardaweel et al., 2015 | Amman, Jordan | Oral contraceptive pill | n=1571
age=18-50 Setting: distributed questionnaire |
Those with experiences of weight gain as a side effect were more likely to possess negative attitudes about OC’s efficacy. Occurrence of side effects was identified as the major reason for discontinuation. Positive attitude towards OC efficacy and safety was associated with their pattern of use. | |||
| Bardaweel et al., 2018 | Jordan | Oral contraceptive pill | n=425
age=18-50 Setting: refugee |
When asked about knowledge, attitude, and experience with hormonal contraceptives, refugee women showed that 60% feared the side effects and 30.6% of those discontinued was due to weight gain. Lack of knowledge of the method correlated with a negative experience with, and negative attitude towards the hormonal contraceptive. | |||
| Belete et al., 2018 | Humera town, Ethiopia | Modern contraceptive (condom, OCP, injectible, IUCD, implant) | n=321
age=15-29 Setting: distributed questionnaire |
This study on married women in Humera Town, Ethiopia revealed that 31.1% of those who experienced side effects discontinued, 34.7% of which was due to weight gain. Majority of the discontinuous responded that the reason for discontinuation was desire to get pregnant, while a major reason for non-use was due to fear of side effects. | |||
| Bhuva et al., 2017 | Pennsylvania, US | LARC, non-LARC | n=987
age=18-40 Setting: distributed survey |
Women who perceived that they were overweight were more likely to choose LARC (over other hormonal methods) than women who perceived normal weight (adjusted ratio showed that there is no association between weight and choice, however). Perception of overweight in women was linked to decreased likelihood of DMPA us age due to weight concern. |
|||
| Chernick et al., 2015 | New York,US | Injectable (depo) IUD, intravaginal ring, implant, patch, pills | n=14
age=14-19 Setting: emergency department |
Interviews showed that barriers of contraception use regarding weight included: Concerns about getting “fat”, Negative attitude because of past experience, Previous contraceptive method changed their body, and causes “bloating”. The subjects eng aged in non-use or inconsistent use of contraceptives while being sexually active. Those with a previous negative experience showed mistrust and were unwilling to try contraception again. |
|||
| Chipeta et al., 2010 | Mangochi district, Malawi | Family planning (pills, condoms, loop, injections) | n=1115
age=15-65 Setting: focus groups in south Malawi |
Depo-provera was the most common modern method used, and included in the reported reasons for non-use of depo included fear of weight gain and obesity. Oral contraceptives were also common. Negative attitudes, myths, and beliefs were present among females in regards to modern contraceptives due to its possible dam age to organs. |
|||
| Clare et al., 2016 | New York, US | Depo, LARC (copper IUD, implant rods) | n=**
age=13-21 Setting: Adolescent Clinic of Metropolitan Hospital Center |
Survey taken at the Adolescent Clinic of Metropolitan Hospital Center revealed weight gain as a common concern for young adults using depo and LARC. Early adults were also concerned about privacy from parents about their contraceptive habits. These concerns can serve as a major barrier to contraceptive use. | |||
| Coombe et al., 2016 | Australia, USA, New Zealand, Japan, Canada, Western Europe | LARC | n=30
age=18-23 Setting: systematic review on developed countries |
The systematic review noticed the prevalence of weight gain as a negative quality. Gubrium 2011 described the impact of women’s fear of side effects and Glasier et al 2008 reported that fear of side effects as well as hearing of other’s experiences can impact. There was also a general trend of increased familiarity of a method increasing attitude towards the method. | |||
| Da Silva et al., 2016 | Brazil, Argentina, Columbia, Mexico | IUD | n=1953
age=20-30 Setting: nursing and medical market research panel |
Of those who attended the nursing and medical market research panel, the questionnaire examined that perceived weight gain was reported by 38.2% of LGS IUS users and 14.3% of copper IUD users. Those from higher education placed value on anecdotal information of healthcare providers. There was an overestimation of risk which prohibited use of the most effective method for them due to their misperceptions. | |||
| Dansereau et al., 2017 | Chiapas, Mexico | Family planning methods (implants, pills, injectables, condoms) | n=292
age=not stated Setting: focus group discussion |
In the study, most participants agreed on the importance of family planning, but many also knew of those who were opposed to it. Both men and women had concerns about short- and long-term side effects of hormonal methods such as pills and injections, one of which was weight gain. A woman expressed her fear towards pills and injectables could possibly kill her, and that she would rather conceive than die of these methods. | |||
| Dickerson et al., 2013 | South Carolina, US | LARC (IUD, SDI) | n=132
age =18 Setting: Medical University of South Carolina (MUSC) family medicine resident and faculty clinics |
A survey of satisfaction, continuation, side effects of LARC found that discontinuation due to weight gain was 20% for SDI and 18.2% for IUD. More overweight and obese women reported weight gain than women of normal body weight. | |||
| Duvan et al., 2010 | Turkey | implant | n=61
age=22-41 Setting: Obstetrics and Gynecology Department of Fatih University, Medical School, |
The study found that the combination of weight gain and anxiety was the second most common reason for discontinuation of Implanon. Weight gain was reported by 10 patients (16%), weight gain and headache by two (3.2%), and weight gain and anxiety by two (1.6%). | |||
| Fait et al., 2018 | Czech Republic, Poland, Romania, Russia, Slovakia | Oral contraceptive | n=615
age≥25 Setting: face-to-face surveys performed by experiences individuals |
A survey of women from countries in Central and Eastern Europe found that 61% of women established positive views of OC when it did not cause weight gain. High proportion of women perceiving weight gain and 65% of women admitted they are worried about weight gain. When asked about OC’s most important feature, 34% responded OC’s no effect on body weight. | |||
| Fruzzetti et al., 2016 | Italy | Pills, vaginal ring | n=1809
age=14-42 Setting: Outpatient clinic of Santa Chiara Hospital |
The survey of attendants at an outpatient clinic in Italy observed 4.8% of women who discontinued due to weight gain and majority of the participants who observed weight gain were unable to quantify their statement. | |||
| Ghule et al., 2015 | Maharashtra, India | oral contraceptive pill | n=62
age=15-24 Setting: in-depth interviews and focus groups |
This qualitative study noticed fear of side effects of oral contraceptive pills when the husband reported their female partner’s fear of weight gain as a reason for her discontinuation. | |||
| Gomez & Freihart, 2017 | US | IUD | n=730
age=18-24 Setting: online survey |
432/730 of the surveyed women were not interested in getting the IUD because of health related fears, which included weight gain. Fears and concerns were noticed in participants who responded that they did not want an IUD. 124 subjects who responded that they were uninterested in ever getting an IUD displayed negative perception of the device, often citing social influences who shared with them their own negative experiences. | |||
| Gómez- Sánchez & Pardo, 2010 | Bogotá, Columbia | Combined oral contraceptives (Injection, oral contraceptive, IUD, implants) | n=12
age=18-45 Setting: proctored discussion in focused groups |
A group of participants in the discussions stated all hormonal contraceptives produce side effects that are “unpleasant” which include weight gain. Others have stated that injectables can induce weight gain and that no weight change is optimal in hormonal contraceptives. When there is a perceived weight change though, participants stated that it could create fear or rejection in women through altering their bodies. | |||
| Hall et al., 2016 | Michigan, US | LARC (IUD, implant) | n=1982
age≥18 Setting: college campus |
This study noticed that when women were asked whether they were worried about the side effect of IUDs, 27.6% identified it as a barrier and 1.9% as a main reason for non-use. When asked the same question about implants, 24.9% identified it as a barrier and 2.6% as a main reason for non-use. The sample showed low understanding of the actuality of LARC’s side effect of weight gain. The study generally noticed that misperception and negative perception can derive from lack of knowledge. | |||
| Hall 2012 | New York City, US | Oral contraceptive | n=354
age=13-24 Setting: university-affiliated community-based clinic in New York City |
This article found that 57% of their subjects reported weight change after 6 months (68% of which was weight gain). They noticed that those with depressed mood are twice more likely to report perceived mood and weight change compared to those without depressed mood. Young women who saw weight changes after 6 months of oral contraceptive use were 40% less likely to continue OC than without weight change. They claimed that perception of weight side effects can serve as a barrier to a contraceptive method. | |||
| Hall et al., 2013 | New York City, US | Oral contraceptive | n=354
age=13-24 Setting: university-affiliated community-based clinic in New York City |
This study found that while 57% of their subjects reported weight change after 6 months (68% of which was weight gain), the majority responded that weight change was “bad” and that weight change was attributed to the pill. They reported that weight change was associated with lower continuation rate, and the reported weight changes, weight gain, “a lot” of weight change was associated with lower continuation rate. | |||
| Hincapié- García et al., 2013 | Madellín, Columbia | Hormonal contraception | n=353
age=17-30 Setting: University of Antioquia |
A survey of University-level women in Columbia found that oral contraceptives were most commonly used, and that incidence of adverse events (48.6%) were associated with hormonal contraceptive discontinuation. Among those adverse events, weight gain (14.5%) and headaches (21.1%) were most prevalent. | |||
| Huda et al., 2014 | Dinajpur, Bangladesh | Norplant | n=73
age=25-31 Setting: Family Planning Association of Bangladesh |
A questionnaire on Bangladesh Norplant users found weight gain (4.1%) as one of the reasons for early removal. 42% of the women were not informed of all of the disadvant ages by their providers when choosing Norplant. The study also found that Norplant users may not have established trust with their providers as shown by the number of Norplant users who consulted with their husbands, family planning workers (31%), Norplant users (11%), and doctors (6.6%) for Norplant insertion. |
|||
| Ibrahim et al., 2015 | Kano, Nigeria | Hormonal contraception | n=334
age=3.72±3.2 setting=Murtala Muhammed Specialist Hospital antenatal care clinic |
This article found that grand multiparous women in Nigeria most commonly used oral contraceptives and injectables. Major reasons for non-use, however, was cited as fear of side effects by 77.2% and desire for more children by 73.1%. Among the feared side effects included weight gain by 83.8%. | |||
| Kucuk et al., 2012 | Aydin, Turkey | Combined oral contraceptive pills | n=418
age=18-49 Setting: Adnan Menderes University Hospital outpatient clinic |
Interviews of Turkey women found that while 68.4% has never tried combined oral contraceptive pills (COCP), 45.2% of the participants believed in its cause of weight gain and 27.5% responded unsure about its effects on weight gain. While other studies have not shown much difference in weight gain from OCP and placebo, this study has shown the prevalence of misconception on COCP’s cause of weight gain in Turkey women. | |||
| Lo & Fan, 2010 | Hong Kong, China | Combined oral contraceptive | n=1295
age=18-45 Setting: online survey |
An online survey of Hong Kong women found that among the 65% of women who have never tried combined oral contraceptives, 72.1% cited fear of side effects (including weight gain) as their primary reason. Similar pattern was examined among those who has discontinued their use of COC, with 27.9% citing the reason for discontinuation as weight gain. | |||
| Manharaj, 2012 | KwaZulu-Natal, South Africa | Family planning methods | n=16 focus groups
age=N/A setting= health facilities |
This study found that South African women were afraid of weight gain because they have noticed acquaintances who appeared overweight after starting contraception. Other women reported discontinuing due to perceived weight gain. It was generally seen that unhappiness can result from severe side effects (weight gain). | |||
| Manzouri et al., 2010 | Isfahan, Iran | IUD | n=11
age=15-49 setting= urban health center |
The interviews from this study found that a common reason for non-use of IUDs was fear of side effects, including weight change. A participant answered that she has heard of IUD causing weight change and did not want that for herself as her husband would not like it. The study noticed that rumors and misperceptions about IUDs came from other IUD users. | |||
| Marvi & Howard, 2013 | Karachi, Pakistan | Pill, injection, IUD | n=20
age=25-45 setting=Rana Liaquat Craftsman Colony health center |
It was found that women believed in the heating effects of contraceptives, which in turn caused weight gain, menstrual irregularities, and weakness. Of the women who had used contraceptives, they also mentioned discontinuing or changing methods due to side effects. The study found that weight gain was thus associated with weakness and irregular bleeding. | |||
| Morotti et al., 2017 | Italy | Nuvaring | n=21
age=18-35 setting=clinic |
This study found that lean, young women on Nuvaring saw a very slight decrease in the aver ages of “satisfaction in body” and “feeling well with their own silhouette.” Neither of these changes were statistically significant. The study also noticed that women perceived feminine figures as most attractive. No one discontinued from the method during the 6 month study. |
|||
| Nanda 2018 | Nairobi, Kenya | LARC (LNG-IUS) | n=29
age=18-49 setting=Family Health Options Kenya clinic |
This article found that women chose LNG-IUD because they perceived that it would have less side effects such as weight gain. One of the participants perceived that there was less hormone and that hormones were localized in the cervix, thus not causing weight gain. Another participant was satisfied with the lack of weight gain after switching from another method that perceived weight gain. | |||
| Nault et al., 2013** | Missouri, US | LARC | n=1146
age=14-45 setting=university-based clinic, abortion clinics, community-based clinics |
Women who received counselling about LARC followed up after their us age and 41% implant and 46% DMPA perceived weight change. Black race, lower SES, higher baseline BMI was associated with perceived weight gain. It was also found that implant and DMPA users were more likely to perceive weight gain than copper IUD users. |
|||
| Ochako et al., 2015 | Kenya | Modern contraceptive methods | n=34
age=16-24 setting=at homes |
This study found in young women that weight change was cited as one of the most common fears of side effects. One of the women interviewed mentioned her belief on how injectables are bad because they make a lot of people notably fat. Study also noticed that 36% women reported discontinuation from the method during their first 12 months due to side effects. | |||
| Vogt & Schaefer, 2012 | Germany | Oral contraceptives | n=51
age=18-24 setting=questionnaire |
This study noticed women’s negative association with weight gain with regard to COC. Women overestimated the risk of, and underestimated effectiveness of COC and many were even concerned about possible weight gain. The study also discovered that even physicians wrongly answered questions about common COC misperceptions. | |||
| Weisberg et al., 2013 | Australia | Hormonal contraceptive | n=200
age=18-50 setting=online survey |
An online survey of women and general practitioners in Australia found that least attractive features of hormonal contraceptives include: weight gain of 3kg; painful, heavy, and irregular periods; high cost; and low failure rates. | |||
| Williamson et al., 2009 | Scotland | LARC | n=20
age=20 setting=homes |
The interview conducted in this study found that the 4 out of 20 interviewed have tried progestin-only-pill or injections and all have discontinued due to experienced side effects. One of the participants noticed weight gain in her friend from injections, and thus did not want to use it herself. Women who were on injectables noticed substantial weight gain and thus cited weight gain as a reason for discontinuation. | |||
Negative Perceptions of Weight Gain
Negative perceptions, defined as knowledge, attitude, or beliefs regarding HC, were reported in thirty-four studies. Knowing someone with a negative experience was also reported to significantly influence acceptance of a given HC method. (5-11) Studies reported that women with negative perceptions were less likely to adhere, thereby reducing a method’s efficacy. (12) Many women stated weight gain was an undesirable side effect of HC methods. (13-22) Women preferred to avoid factors that changed their bodies and viewed them negatively. (23, 24) Among those who used oral contraceptives, 34% (N=615) noted that no effect on weight was the most important feature of their oral contraceptive choice, and 46% (N=615) of women stated that weight gain was the side effect they were most concerned about. (25).
Twelve articles discussed the fear of weight gain. Women feared weight gain as a side effect, perceiving it as undesirable and harmful. (20, 23, 26) Fear of gaining weight was noted as a top reason for women's non-use or discontinuation of HC. (7, 9, 19, 21, 27-29) For example, among Northern Nigerian women, the most significant contributor (77.2%, N=334) in the non-use of HC methods was the fear of side effects; of which 83.8% (N=334) perceived weight gain as a side effect. (28)
Four studies examined how women's negative perception of weight gain from HC methods was related to obesity concerns. Obesity was cited as a feared side effect for some women, which contributed to their non-use of injectable methods. (7) In general, women who perceived themselves as overweight or obese were conscious of how their contraceptive decision affected their body weight. (30) Women with these perceptions were more likely to choose LARCs over injectable methods or avoid either method altogether. (30) Furthermore, while using LARCs, overweight or obese women reported more weight gain perception than women with normal weight. (31, 32)
Twenty-two articles discussed the avoidance of HC due to weight gain concerns. Many women cited weight gain as their main reason for avoidance. (7, 8, 10, 21, 27, 28, 30, 33-36) Women wanted to avoid methods they believed caused weight gain, even if not scientifically proven.
Discontinuation was the most common result of weight gain-related perceptions. After six months, women who reported weight changes were less likely to continue their oral contraceptive methods. (16) This was especially true if women perceived drastic weight changes. (17) Contraceptive discontinuation was also influenced by combined side effects such as weight gain and anxiety or headache. (11, 18, 31, 37-41)
Misperceptions or Limited Contraceptive Knowledge
Seventeen studies concluded that women received incomplete counseling regarding the side effects of HC. Lack of counseling influenced decision making, weighted by fear of side effects, such as potential weight gain. In a South African study, women reported that their providers merely gave suggestions on a contraceptive method rather than providing comprehensive information to make their own decisions. (10) A study on university women in Colombia concluded that 41.4% (N=353) of women thought contraceptive counseling was lacking. (18) Women in rural Mexico demonstrated awareness of a HC method but insufficient knowledge due to ineffective counseling. (26) In the US, the underuse of LARCs is related to a lack of awareness or knowledge from potential users and clinicians. (31)
Women relied on personal relationships such as friends and family, who often provided misinformation, when contraceptive counseling fell short. (21) Ibrahim and Rabiu also noted that women cited nurses, midwives or the media as their primary sources of information, indicating that effective counseling does not stem only from physician providers. Moreover, inadequate counseling of side effects is a significant predictor of discontinuation. (28, 38) Accordingly, women who were better informed about the implants' expected side effects were more likely to continue with the method. (39) Thus, contraceptive counseling can be imperative to awareness of options and knowledge of HC methods and associated side effects; it can also influence satisfaction with the chosen method and trust in providers. (9, 12, 22, 24, 29, 40, 42)
Fifteen articles demonstrated that a lack of contraceptive knowledge was the reason for perceiving or predicting weight change when using a HC. Contraceptive knowledge includes information about proper use, mechanism, efficacy, advantages, and side effects. Lack of knowledge resulted in overestimation of the risks and underestimation of the benefits associated with HC, and correlated with negative experiences in general. (37,43)
Women’s educational level, self-reported in surveys, interviews, and focus groups, was established as the reason why some women were not knowledgeable of HC methods. (6, 8, 14) However, da Silva-Filho found that higher education does not correlate with better contraceptive knowledge. Women with higher education (more than 12 years) overestimated risk, similarly to women without higher education, and emphasized anecdotal information instead of healthcare providers' recommendation. (8) A study in Turkey found that misconception of combined oral contraceptive pills (COCPs) was prevalent, 45.2% (N=418) believed that COCPs cause weight gain, and 27.5% were unsure if COCPs caused significant weight gain. (29)
Discussion
The findings of this review indicate that negative perceptions of weight gain from HC may influence women’s contraception decisions. As Lopez et al. established, most HC methods lack scientific consensus to determine their causal role in actual weight gain. This is consistent with a study done by Beksinska, where clients commonly perceived weight gain from HC methods even when actual weight gain has not been associated with the method in scientific studies. (44) This review reported that while there is not a consensus to validate the causation of weight gain from HC methods, women consistently discontinue their hormonal methods due to perceived weight gain. (44) Beksinska and Smit also noted that healthcare providers themselves might harbor negative perceptions of these methods, affecting prospective users. (44)
Women reported perceived weight gain as a negative side effect of most HC methods, although limited evidence exists to prove such a theory. (1) Informational websites, packaging, and organizations such as the American Family Physician, often list weight gain as a side effect and include it in counseling users. (45) As the data is inconclusive regarding weight gain as a side effect, there is misinformation and confusion surrounding this. Information provided on contraception labels and during contraceptive counseling can negatively shape women's perceptions even if the possibility of gaining weight due to the method is low.
The studies found that women mainly learned about side effects of contraception from first and second-hand experiences rather than health professionals. Many women did not receive counseling or were given false information regarding the HC method and weight change (I.e. this method does not cause weight gain). Weight gain was often cited as the top side effect of HC, and such negative experiences often outweighed the benefits of pregnancy prevention. Misinformation plays a role in a woman's decision to discontinue HC. Although we recognize that many women may not have conversations with their providers regarding misconceptions, it may be worth investing in a patient centered reproductive justice framework to dispel some of these myths. Paying special attention to people of color and other marginalized communities who may have experienced historical and ongoing reproductive mistreatment could make a significant difference in these perceptions among women.
Citing perceived weight gain as a primary reason for discontinuation indicates that negative perception or misinformation affects women's satisfaction. Whether women are gaining weight or not, the perception of gaining weight is a significant indicator of utilization. A woman's perception of her weight while using HC methods is equally as important as the number on the scale regarding satisfaction and continuation of a HC method. (32) Women with negative experiences with HC Generator methods were less likely to use contraceptives again. (13, 23) Some women frequently changed HC methods because they believed they were gaining weight.
Women with obesity concerns may prioritize weight maintenance over effective family planning methods. Women who perceived themselves as obese were more inclined to avoid or choose certain hormonal contraceptives. These decisions stemmed from the perception that some methods, such as injectable HC, caused more weight gain over others (for example, LARC), or that no method prevents weight gain. Thus, even if women were not obese, these perceptions are enough to influence their contraceptive decision. Women who are concerned about obesity are predisposed to perceiving weight gain for any reason. This may bias women’s perception that actual weight gain occurred, leading to discontinuation of HC methods. (31, 32) Also, those concerned with their weight may be more sensitive to any perceived changes. Healthcare providers need to be considerate of weight or obesity concerns when discussing hormonal methods.
Mismatched HC method information was another theme that arose from the literature, causing women to believe myths about HC methods and weight gain. (44) There are various reasons why women do not have proper knowledge of HCs. Women report that information provided during HC counseling often does not align with the information they want to know, further contributing to discontinuation or utilization. Women's educational level may play a part as limited education could be correlated to living in poor or medically underserved regions. Women in these areas may be more susceptible to misconceptions. Nonetheless, women with higher education may also harbor misconceptions based on anecdotal information from peers. (8) The prevalence of weight gain misperceptions explains why a woman might think she is gaining weight while using a HC method.
While women were informed about HCs efficacy for family planning, misinformation on its side effects served as a prominent barrier to HC usage. Healthcare providers' awareness of negative perceptions may be useful in approaching conversations about perceived side effects. Providers could eliminate misconceptions about the risk of weight gain through counseling to create more positive experiences for women using a HC method. Improved counseling was shown to reduce the rate of unwanted pregnancy in populations that included women from racially and socioeconomically diverse backgrounds. (42) By clarifying the misbelief surrounding weight gain, women worldwide may be less likely to discontinue the use of a HC method and practice healthy family planning methods.
This literature review found six overarching themes relating to negative perceptions of hormonal contraceptives and weight gain, which could instill non-acceptance towards the method. Understanding women's perception of hormonal contraceptives can facilitate appropriate conversations based on women's concerns. As hormonal contraception becomes more accessible to women, the next step includes increasing continuation rates and satisfaction.
Limitation
This review examined open-access, peer-reviewed studies observing the relationship between hormonal contraception and perceived weight change. Limitations may exist because the 39 reviewed articles did not cover all available hormonal contraceptive methods in-depth since a frequent focus of available articles was on oral contraceptives. Actual reports of weight gain were excluded, even if self-measured, due to the chance that perceptions could be altered. The exclusion of actual weight is a limitation as it significantly reduced the articles available for review and may present a perspective missing in our data. Additionally, some articles were excluded if they could not be translated into English, and sample sizes varied among the studies making the conclusions difficult to generalize across groups.
Conclusion
Women need improved hormonal contraception counseling from a healthcare professional when deciding on a HC method that best fits their needs. Understanding women’s perception of hormonal contraceptives can facilitate appropriate conversations to personalize contraceptive usage based on individual concerns. Since hormonal contraception plays a relevant role in women’s sexual health, next steps include improving HC continuation rates and increasing satisfaction. This study indicates that while there isn’t scientific consensus on weight gain causation from contraceptive methods women are in need of hormonal contraception counseling that dispels existing misinformation regarding the risk of weight gain with HC use. Women often perceive that HC counseling does not address their concerns about side effects, including weight gain. The next step to address these issues may be to develop patient centered HC counseling resources for providers to improve women’s acceptance and satisfaction using HC.
Conflicts of Interest
None declared.
Acknowledgment
We would like to thank Nathalie Zamora and Alia Ortiz, who participated in the initial data collection process.
References
- Gallo, M.F., et al., Combination contraceptives: effects on weight. Cochrane Database of Systematic Reviews, 2014(1).
- Lopez, L.M., et al., Progestin-only contraceptives: effects on weight. Cochrane Database of Systematic Reviews, 2011(4).
- Daniels, K. and J. Jones, Contraceptive methods women have ever used: United States, 1982-2010. 2013: US Department of Health and Human Services, Centers for Disease Control and ….
- Fryar CD, Carroll MD, Ogden CL. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2015–2016. 2018.
- Agasti N, Mohapatra G, Behera TR, Mohanty S. ASSESSING THE KNOWLEDGE AND PRACTICE OF HEALTH WORKER FEMALE ON DIFFERENT FAMILY PLANNING METHODS IN ORISSA. Journal of Evolution of Medical and Dental Sciences-Jemds. 2017;6(55):4154-6.
- Al-Mass AA, Al-Shahrani BS, Al-Mweisheer AN, Tulbah SA, Syed S, Anwer R, et al. User Experience, Knowledge and Practice of Oral Contraceptive: A Study from Riyadh, Saudi Arabia. Annals of Medical and Health Sciences Research. 2018;8(6):411-
- Chipeta EK, Chimwaza W, Kalilani-Phiri L. Contraceptive knowledge, beliefs,and attitudes in rural Malawi: misinformation, misbeliefs,and misperceptions. Malawi medical journal : the journal of Medical Association of Malawi. 2010;22(2):38-41.
- da Silva AL, Lira J, Rocha ALL, Ferreira MCF, Lamaita RM, Candido EB, et al. Non-hormonal and hormonal intrauterine contraception: survey of patients' perceptions in four Latin American countries. European Journal of Contraception and Reproductive Health Care. 2016;21(3):213-9.
- Gomez A, Freihart B. Motivations for Interest, Disinterest and Uncertainty in Intrauterine Device Use Among Young Women. Maternal & Child Health Journal. 2017;21(9):1753-62.
- Maharaj P. Stalling contraception? Perspectives and experiences of sexually active women and men. Agenda. 2012;26(2):100-
- Williamson LM, Buston K, Sweeting H. Young women's continued use of oral contraceptives over other hormonal methods: findings from a qualitative study. The journal of family planning and reproductive health care. 2009;35(3):167-72.
- Bardaweel SK, Akour AA, Kilani M-VZ. Current knowledge, attitude, and patterns of oral contraceptives utilization among women in Jordan. BMC Womens Health. 2015;15.
- Coombe J, Harris ML, Loxton D. What qualities of long-acting reversible contraception do women perceive as desirable or undesirable? A systematic review. Sexual health. 2016;13(5):404-19.
- Ghule M, Raj A, Palaye P, Dasgupta A, Nair S, Saggurti N, et al. Barriers to use contraceptive methods among rural young married couples in Maharashtra, India: Qualitative findings. Asian journal of research in social sciences and humanities. 2015;5(6):18-
- Gómez-Sánchez PI, Pardo Y. Percepciones del uso de anticonceptivos en Bogotá(Colombia) 2009: Estudio cualitativo. Revista Colombiana de Obstetricia y Ginecología. 2010;61(1):34-41.
- Hall KS, White KO, Rickert VI, Reame N, Westhoff C. Influence of depressed mood and psychological stress symptoms on perceived oral contraceptive side effects and discontinuation in young minority women. Contraception. 2012;86(5):518-25.
- Hall KS, White KOC, Rickert VI, Reame NK, Westhoff CL. An Exploratory Analysis of Associations Between Eating Disordered Symptoms, Perceived Weight Changes, and Oral Contraceptive Discontinuation Among Young Minority Women. Journal of Adolescent Health. 2013;52(1):58-63.
- Hincapié-García JA, Quintero-Agudelo M, Gaviria J, Estupiñán-Cabrera H, Amariles P. Causas de abandono, cambio o fallo terapéutico de la anticoncepción hormonal en mujeres universitarias. CES Medicina. 2013;27(2):153-62.
- Lo SS, Fan SY. Acceptability of the combined oral contraceptive pill among Hong Kong women. Hong Kong medical journal = Xianggang yi xue za zhi. 2016;22(3):231-6.
- Marvi K, Howard N. Objects of temporary contraception: an exploratory study of women's perspectives in Karachi, Pakistan. BMJ open. 2013;3(8).
- Ochako R, Mbondo M, Aloo S, Kaimenyi S, Thompson R, Temmerman M, et al. Barriers to modern contraceptive methods uptake among young women in Kenya: a qualitative study. BMC public health. 2015;15:118.
- Weisberg E, Bateson D, Knox S, Haas M, Viney R, Street D, et al. Do women and providers value the same features of contraceptive products? Results of a best-worst stated preference experiment. The European journal of contraception & reproductive health care : the official journal of the European Society of Contraception. 2013;18(3):181-90.
- Chernick LS, Schnall R, Higgins T, Stockwell MS, Castaño PM, Santelli J, et al. Barriers to and enablers of contraceptive use among adolescent females and their interest in an emergency department based intervention. Contraception. 2015;91(3):217-25.
- Manzouri L, Aghdak P, Nematollahi S, Mansouri A, Aghababaeian A, Nasiri SDND. Misbelieves about Intra Uterine Device (IUD) in Isfahan, Iran. Journal of Family and Reproductive Health. 2010:169-74.
- Fait T, Buryak D, Cirstoiu MM, Luczai E, Janczura R. Needs,and preferences of women users of oral contraceptives in selected countries in Central and Eastern Europe. Drugs in context. 2018;7:212510.
- Dansereau E, Schaefer A, Hernandez B, Nelson J, Palmisano E, Rios-Zertuche D, et al. Perceptions of and barriers to family planning services in the poorest regions of Chiapas, Mexico: a qualitative study of men, women, and adolescents. Reprod Health. 2017;14(1):129.
- Bajwa SK, Bajwa SJS, Ghai GK, Singh K, Singh N. Knowledge, Attitudes, Beliefs, and Perception of the North Indian Population Toward Adoption of Contraceptive Practices. Asia-Pacific Journal of Public Health. 2012;24(6):1002-12.
- Ibrahim G, Rabiu A, Abubakar IS. Knowledge, attitude and practice of contraceptives among grand multiparous women attending antenatal clinic in a specialist hospital, Kano, Nigeria. Nigerian Journal of Basic & Clinical Sciences. 2015;12(2):90-4.
- Kucuk M, Aksu H, Sezer SD. Misconceptions about the side effects of combined oral contraceptive pills. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology. 2012;28(4):282-5.
- Bhuva K, Kraschnewski JL, Lehman EB, Chuang CH. Does body mass index or weight perception affect contraceptive use? Contraception. 2017;95(1):59-64.
- Dickerson LM, Diaz VA, Jordon J, Davis E, Chirina S, Goddard JA, et al. Satisfaction, early removal, and side effects associated with long-acting reversible contraception. Fam Med. 2013;45(10):701-7.
- Nault AM, Peipert JF, Zhao Q, Madden T, Secura GM. Validity of perceived weight gain in women using long-acting reversible contraception and depot medroxyprogesterone acetate. Am J Obstet Gynecol. 2013;208(1):48.e1-8.
- Altaf EW, Hebert LE, Newton SL, Gilliam M. “Counting calories and hooking up”: examining body image and sex without birth control among college women. Contraception. 2017;96(4):291-.
- Hall KS, Ela E, Zochowski MK, Caldwell A, Moniz M, McAndrew L, et al. "I don't know enough to feel comfortable using them:" Women's knowledge of and perceived barriers to long-acting reversible contraceptives on a college campus. Contraception. 2016;93(6):556-64.
- Morotti E, Casadio P, Guasina F, Battaglia B, Mattioli M, Battaglia C. Weight gain, body image and sexual function in young patients treated with contraceptive vaginal ring. A prospective pilot study. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology. 2017;33(8):660-4.
- Nanda G, Rademacher K, Solomon M, Mercer S, Wawire J, Ngahu R. Experiences with the levonorgestrel-releasing intrauterine system in Kenya: qualitative interviews with users and their partners. The European journal of contraception & reproductive health care : the official journal of the European Society of Contraception. 2018;23(4):303-8.
- Bardaweel SK, Akour AA, Alkhawaldeh A. Impediments to use of oral contraceptives among refugee women in camps, jordan. Women & Health. 2018.
- Belete N, Zemene A, Hagos H, Yekoye A. Prevalence and factors associated with modern contraceptive discontinuation among reproductive age group women, a community based cross-sectional study in Humera town, northern Ethiopia. Bmc Womens Health. 2018;18(1):190.
- Duvan CI, Gözdemir E, Kaygusuz I, Kamalak Z, Turhan N. Etonogestrel contraceptive implant (Implanon): analysis of patient compliance and adverse effects in the breastfeeding period. Journal of the Turkish-German Gynecological Association. 2010;11(3):141-4.
- Fruzzetti F, Perini D, Fornaciari L, Russo M, Bucci F, Gadducci A. Discontinuation of modern hormonal contraceptives: an Italian survey. The European journal of contraception & reproductive health care : the official journal of the European Society of Contraception. 2016;21(6):449-54.
- Huda FA, Chowdhuri S, Sirajuddin MFR. Importance of Appropriate Counselling in Reducing Early Discontinuation of Norplant in a Northern District of Bangladesh. Journal of Health Population and Nutrition. 2014;32(1):142-8.
- Clare C, Squire M-B, Alvarez K, Meisler J, Fraser C. Barriers to adolescent contraception use and adherence. International Journal of Adolescent Medicine & Health. 2018;30(4):1-8.
- Vogt C, Schaefer M. Seeing things differently: Expert and consumer mental models evaluating combined oral contraceptives. Psychology & Health. 2012;27(12):1405-25.
- Beksinska ME, Smit JA, Guidozzi F. Weight change and hormonal contraception: fact and fiction. Expert Review of Obstetrics & Gynecology. 2011;6(1):45-56.
- Physician AF. Side Effects of Hormonal Contraceptives 2010 [Available from: https://www.aafp.org/afp/2010/1215/p1509.html.]

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.