Case Report
Depression and Anxiety as Important Aggravating Factors of Pain in Morton’s Neuroma: A Case Report
Golale Modarresi1, Shirin Modarresi2
Published online: September 10 2021
1Bridgepoint Collaboratory for Research and Innovation, Lunenfeld-Tanenbaum Research Institute, Sinai Health, Toronto, Ontario, Canada
2School of Physical Therapy, Western University, London, Ontario, Canada
Corresponding Author: Shirin Modarresi, email smodarre@uwo.ca
DOI: 10.26443/mjm.v20i2.884
Abstract
This report represents a case of Morton’s neuroma with episodic severe pain in the forefoot. Initially, the patient was prescribed naproxen 500 mg twice per day, anti-inflammatory topical cream, and massage. In a follow up visit, the patient was still experiencing frequent episodic sharp pain. In a detailed patient interview, it was revealed that she has depression and anxiety and suffers from social isolation, which co-occurred with episodes of severe pain. Therefore, she was referred to a psychologist and a community support group and started practicing body relaxation techniques such as guided imagery and breathing exercises. The new treatment strategy had a major impact on improving her symptoms. This report aims to illustrate that depression and anxiety can be one of the main aggravating factors in conditions that cause episodic pain, as in this case of Morton’s neuroma. Removing psychosocial contributors of pain has the potential to decrease the need for more invasive interventions.
Learning Points
- This study highlights the importance of recognizing psychosocial contributors of pain in a case of Morton's neuroma
- Taking a detailed history is essential to recognize all the potential triggers of pain, even when the disorder has a typical presentation with an identified pathology
- By evaluating and identifying psychosocial contributors, the necessity of painkillers and invasive interventions can subside
Tags: Morton’s neuroma, Pain, Biopsychosocial model
Introduction
Morton's neuroma is one of the most common causes of forefoot pain. (1) It can develop when the tissues and bursa surrounding an interdigital nerve thicken from chronic pressure and lead to swelling or fibrosis around the vessels and the nerve. (2) The resultant neuropathy is mainly due to irritation of the interdigital nerves close to the plantar aspect of the transverse intermetatarsal ligament during dorsiflexion. (2) Common causes include narrow toe-box footwear, high heels, lipoma, joint dislocations, repetitive trauma, or blunt injury. (3)
Morton's neuroma mostly occurs between the third and fourth metatarsals and pain may radiate to other toes, though occurrences between the second and third metatarsals has also been reported. (4) The most common aggravating factor is walking, especially in tight or high-heeled shoes, and the most common relieving factors are resting and taking off footwear. (2) Numbness and night-time awakening pain can happen, (4) and with prolonged activity, pain can radiate to the calf and other parts of the foot as well. (2) The first-line treatment option is supportive care, such as wearing a wide shoe with soft insoles and a low heel that unloads the pressure on the nerve. (2) Nonsteroidal anti-inflammatory drugs, anti-epileptic medications, and tricyclic antidepressants may also be effective. (2) Injection of anesthetics as a gentle invasive treatment is used as second line. (2) Steroid injection is a short-term effective symptom reliever but may cause side effects, including atrophy of the subcutaneous fat, skin thinning, and even deformity. (2) The effectiveness of surgical interventions remains controversial thus, they are usually reserved for when conservative management has failed for at least several months. (3) The CARE guideline was used to guide this case report. (5)
Case report
Patient’s presenting profile: the patient is a 70-year-old female, admitted to the outpatient department, complaining of sharp and severe episodic pain in the tip of the left second distal phalanx. Subjective history revealed an insidious onset that started around seven years ago with no known history of trauma. Since then, the patient has been changing her footwear regularly, as it alleviates her pain. While she has excruciating pain, she notices warmth and visible bulging of the veins on her foot however, denies any numbness, tingling, or cramps. Over the course of two years, her pain has intensified and the periodic events no longer correlate with activity, which was previously an aggravating factor for pain. Nevertheless, she does mention that long walks bring forth a tingling sensation in the forefoot. In order to alleviate her pain, she has been taking over-the-counter medications, including ibuprofen and topical remedies. Unfortunately, these medications have provided no relief. Furthermore, the patient denies wearing tight shoes, and reports performing a mild level of physical activity (i.e., slow-paced walking). The persistent pain has been distressing her, as she expresses feelings of nervousness and hopelessness.
Past medical history: her past medical history consists of hallux valgus correction surgery done on bilateral feet four years ago, with no post-operation complications. She denies wearing high heels for over 45 years. She also reports taking 20 mg of citalopram daily for mild depression for the past fifteen years. The patient denies diabetes, rheumatic diseases, allergies, kidney, liver dysfunction, recreational drugs, alcohol abuse, and any family history of similar type of pain.
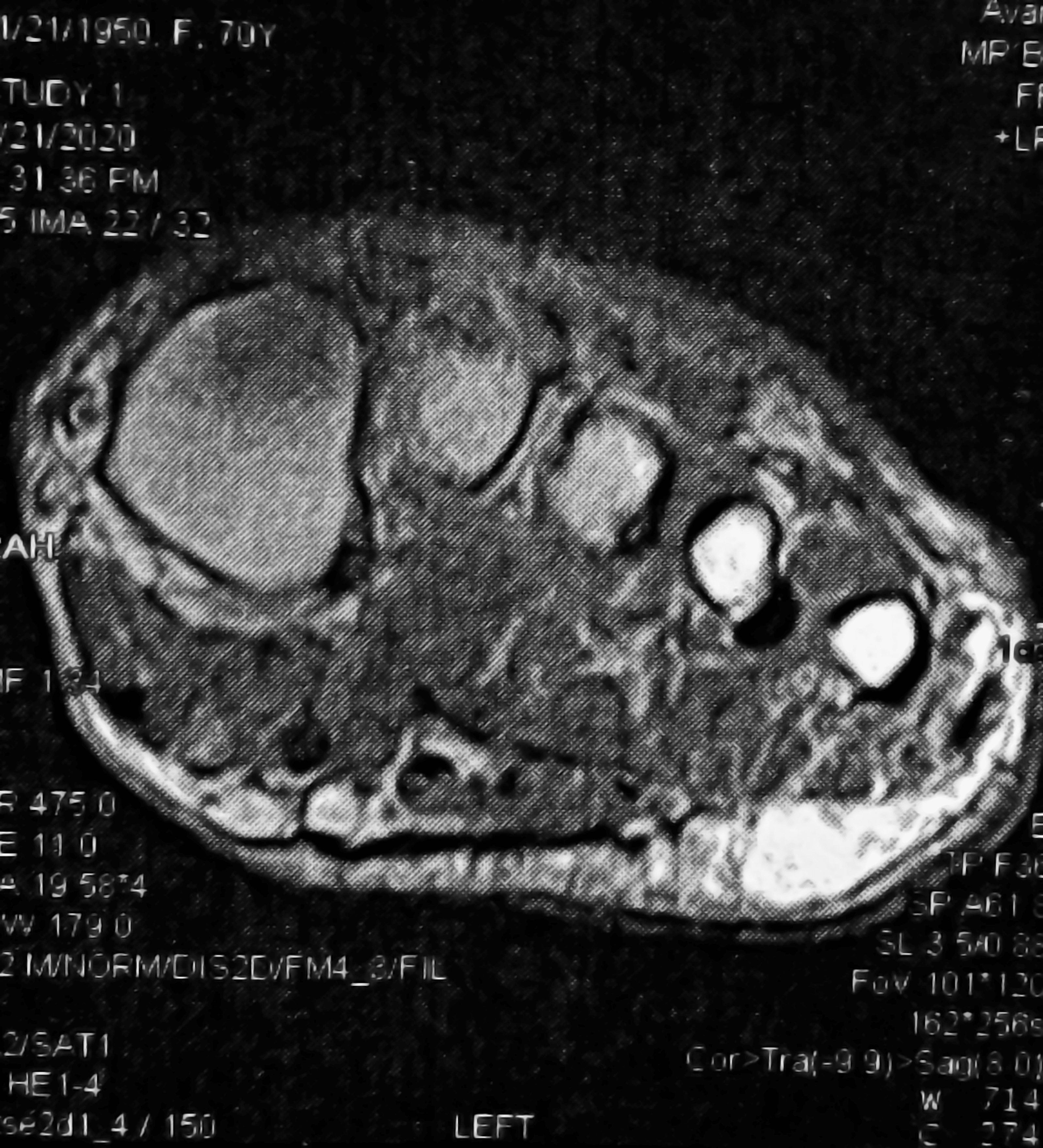
Physical examination: vital signs and body mass index were normal. On inspection, there were no swelling, discoloration, or atrophy at the location of the pain. The shape and color of the nails were normal. There was no warmth, mass, crunching, lump, or clicking. On palpation, save for the second toe, other parts of the left foot had no tenderness. Dorsalis Pedis and Tibialis arteries' pulses, as well as capillary fillings were normal. The dermatomal assessment was symmetrical and unremarkable. The range of motion of the joints were within normal limits. On X-ray, no signs of fracture, injury, or trauma to the second metatarsal and phalanx were visible. On MRI, Morton's neuroma by the second meta-tarsal was detected by a radiologist (Figure 1). The patient rated her pain at 8/10 on the numeric pain rating scale (NPRS). A squeeze test was performed by applying pressure on the dorsal and plantar surface of the second distal meta-tarsal. A Morton's test was conducted in which one hand was placed on the medial side of the patient's foot near the metatarsophalangeal joint, and the other hand was placed on the lateral side, and pressure was applied to squeeze the two sides. The results of both tests were positive with the reproduction of the familiar pain. The patient was advised to use topical salicylate ointment and to gently massage the second and third metatarsals by spreading and mobilizing the metatarsal heads. She was also advised to take 500 mg naproxen, a maximum of two tablets daily.
Psychosocial assessment: Three weeks later, the patient still reported the same amount of pain in a follow-up visit. During this visit, a more thorough patient interview including evaluations of social and psychological factors was conducted. The patient revealed that she suffers from social isolation with no family and social support. In addition, the patient indicated that she has been experiencing anxiety in the past two years, which was concurrent with the severe pain onset. She displayed depression and anxiety symptoms, including nervousness, restlessness, agitation, fatigue, sadness, and loss of interest in activities of daily living (ADLs). According to the patient, her mental health also affects her appetite, ADLs, and sleep quality. Her score on the Hospital Anxiety and Depression Scale was 15/21, depicting presence of depression and anxiety.
Analysis: Upon further investigation, it was revealed that her pain exacerbates at times of severe depression and anxiety. In other words, there was a strong correlation between episodes of pain in the forefoot and when she felt extremely sad and anxious. Based on this finding, she was referred to a psychologist for weekly sessions and a community support group to address her social isolation. In the meantime, she started body relaxation techniques such as guided imagery and breathing exercises on a daily basis (at least one or two times per day). These strategies were in addition to the previously prescribed treatments such as specific massage techniques, naproxen, and topical salicylate ointment. After four weeks, in a follow-up visit, her pain level had decreased to 4/10 on the NPRS, which was controllable by taking 500 mg naproxen a day. The patient’s mental status improved, and she reported a significant decrease in the frequency of painful forefoot episodes.
Discussion
To the authors' knowledge, this is the first case report of a patient with Morton's neuroma having social and psychological factors as the main triggers of pain. This study highlights the necessity for considering these triggers and working towards removing them to not only reduce the need for pharmacological treatments, but also decrease the necessity of invasive interventions. This finding is in line with the biopsychosocial model of pain, which posits that not only tissue pathology contributes to the experience of pain, but that also social and psychological factors play important roles. (6)
Psychological factors such as depression have been reported as significant predictors of chronic pain following an injury. (7) Uncovering the exact underlying mechanism of how psychosocial factors could have affected the experience of pain for this patient is beyond the scope of this paper however, we can offer some explanations. Previous research has shown that people with high levels of anxiety are more sensitive to pain, and stress or other negative emotions are associated with lower pain thresholds. (8) In addition, pain shares some common biological mechanisms with depression and anxiety. For instance, various parts of the brain have vital roles in processing both anxiety and pain such as the periaqueductal gray and anterior cingulate cortex, as both regions get activated while feeling either pain or anxiety. (9) Even the severity of pain and psychological disorders are significantly correlated with each other. (10) This overlap of biological mechanisms can also lead to a vicious cycle between pain and psychological disorders, as pain is a risk factor for developing depression and anxiety. (9) Also, neurotransmitters such as glutamate have shown to play essential roles in regulating both mental health and pain. (9) In addition, emotional disorders might affect pain through other health behaviors such as nutrition and sleep. (7) Therefore, clinicians are recommended to screen for depression and anxiety, especially if the patient suffers from severe chronic pain. Focusing on typical causes and triggers may hinder the clinicians' and the patients' awareness that an underlying psychiatric condition may exist and potentially play a significant role. By going beyond the pathophysiology of a disorder, identifying the psychosocial contributors of pain, and implementing these factors into the management strategy, we can decrease the necessity of painkillers and invasive interventions, and optimize individualized care that is evidence-based and comprehensive.
This case report's principal strength is that it provides a clear example of how psychosocial factors can be the main triggers of pain, in this case for a patient with Morton's neuroma. The main limitation is the inability to create a causal link between depression/anxiety and the episodic periods of pain. Further research is required to establish a definite cause and effect relationship. Informed consent was obtained from the patient for this case report.
References
- Ruiz Santiago F, Prados Olleta N, Tomás Muñoz P, Guzmán Álvarez L, Martínez Martínez A. Short term comparison between blind and ultrasound guided injection in morton neuroma. Eur Radiol. 2019 Feb;29(2):620–7.
- Munir U, Tafti D, Morgan S. Morton Neuroma. In Treasure Island (FL); 2021.
- Jain S, Mannan K. The diagnosis and management of Morton’s neuroma: a literature review. Foot Ankle Spec. 2013 Aug;6(4):307–17.
- Zabaglo M, Dreyer MA. Neuroma. Treasure Island (FL): StatPearls Publishing; 2021.
- Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017 Sep;89:218–35.
- Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007 Jul;133(4):581–624.
- Modarresi S, Suh N, Walton DM, MacDermid JC. Depression affects the recovery trajectories of patients with distal radius fractures: A latent growth curve analysis. Musculoskelet Sci Pract. 2019 Oct;43:96–102.
- Dufton LM, Konik B, Colletti R, Stanger C, Boyer M, Morrow S, et al. Effects of stress on pain threshold and tolerance in children with recurrent abdominal pain. Pain. 2008 May;136(1–2):38–43.
- Bushnell MC, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci. 2013 Jul;14(7):502–11.
- Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain. 1997 Jun;13(2):116–37.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.