Approach To
Shock
Janet Chan1
Published online: 02 February 2022
1Faculty of Medicine, McGill University, Montreal, QC, Canada
Corresponding Author: Janet Chan, email: janet.chan3@mail.mcgill.ca
DOI: 10.26443/mjm.v20i2.872
Abstract
Shock is a life-threatening pathophysiologic state referring to inadequate organ perfusion, which can progress to end-organ dysfunction and eventually, multiple organ failure and death. The diagnosis of shock is clinical, necessitating a good understanding of the underlying etiology, pathophysiology, as well as the clinical, biochemical, and hemodynamic manifestations of the various presentations of shock. This article describes an approach to shock, highlighting the important initial actions, pertinent clinical findings, the four main types of shock, and the mainstays of management including the use of intravenous fluids, inotropes, and vasopressors. A case study and additional figures are included to supplement the presented concepts.
Tags: Shock, Vasopressers, Inotropes, Cardiogenic shock, Neurogenic shock, Obstructive shock, Anaphylactic shock, Hypovolemic shock, Septic shock.
Question
A 54-year-old man was brought to the emergency department overnight following a motor vehicle accident. Although he was found to be neurologically intact, and examination of his head and extremities was largely unremarkable, an ultrasound examination revealed intra-abdominal free fluid. He underwent a laparotomy for a ruptured spleen.
He is otherwise not known for any past medical history (including allergies and alcohol/recreational drug use), and up until last night had been in his usual state of health. There is no notable family history.
The patient’s post-operative recovery course is unremarkable until mid-morning, about 5 hours after his operation. He is found by his nurse to be less responsive, with a blood pressure drop from 136/90 to 89/55, an increase of his heart rate to 121, a temperature of 38.1oC, and increased oxygen needs. On physical exam, his abdomen is soft, dressings are dry, and capillary refill is normal. His skin is warm to touch. His EKG indicates sinus rhythm, unchanged from his baseline. Stat labs are drawn, and first to result is his blood gas lactate, which is elevated from 2 hours ago. He rapidly deteriorates with disseminated intravascular coagulation (DIC).
Which type of shock would you consider most probable in this scenario?
A. Hypovolemic shock
B. Cardiogenic shock
C. Septic shock
D. Anaphylactic shock
E. Neurogenic shock
Answer
C. The most likely diagnosis in this scenario is septic shock. His presentation (fever, vasodilation, DIC) is consistent with septic shock, and the history of abdominal surgery and trauma suggests a potential source of infection: gut organisms introduced into the bloodstream. Although hypovolemic shock should always be strongly considered in trauma and/or surgical cases, this patient’s bleeding appears to have been controlled upon arrival/in the operating room, and there was no overt source of bleeding or fluid loss post-operatively. Furthermore, being in a monitored setting, the patient was likely receiving fluids and/or transfusions.
The patient’s presentation is also less consistent with cardiogenic shock, as the patient has no cardiac history, his ECG is normal, and cardiogenic shock is unlikely to cause DIC. Anaphylactic shock is unlikely, as there is no suspected allergen, and the patient is not known for any allergies. Neurogenic shock is also unlikely, given the unremarkable neurological examination and lack of evidence of head or spinal cord injury, although it can be a cause of DIC. Case adapted from Kaplan Medical (1).
Initial Approach
Shock is a life-threatening pathophysiologic state referring to inadequate organ perfusion, which can progress to end-organ dysfunction and eventually, multiple organ failure and death (2, 3). Shock may arise from increased oxygen demands, impaired delivery of oxygen, impaired utilization of oxygen, or a combination of these processes (3).
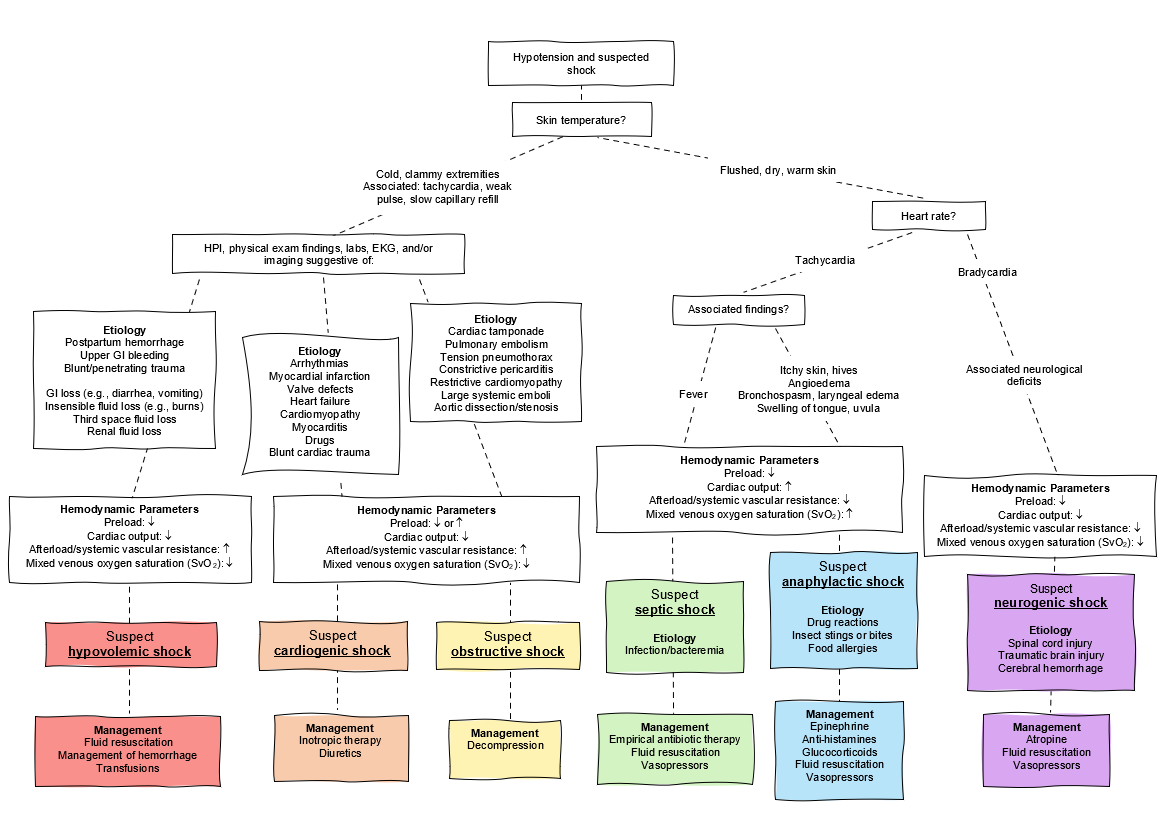
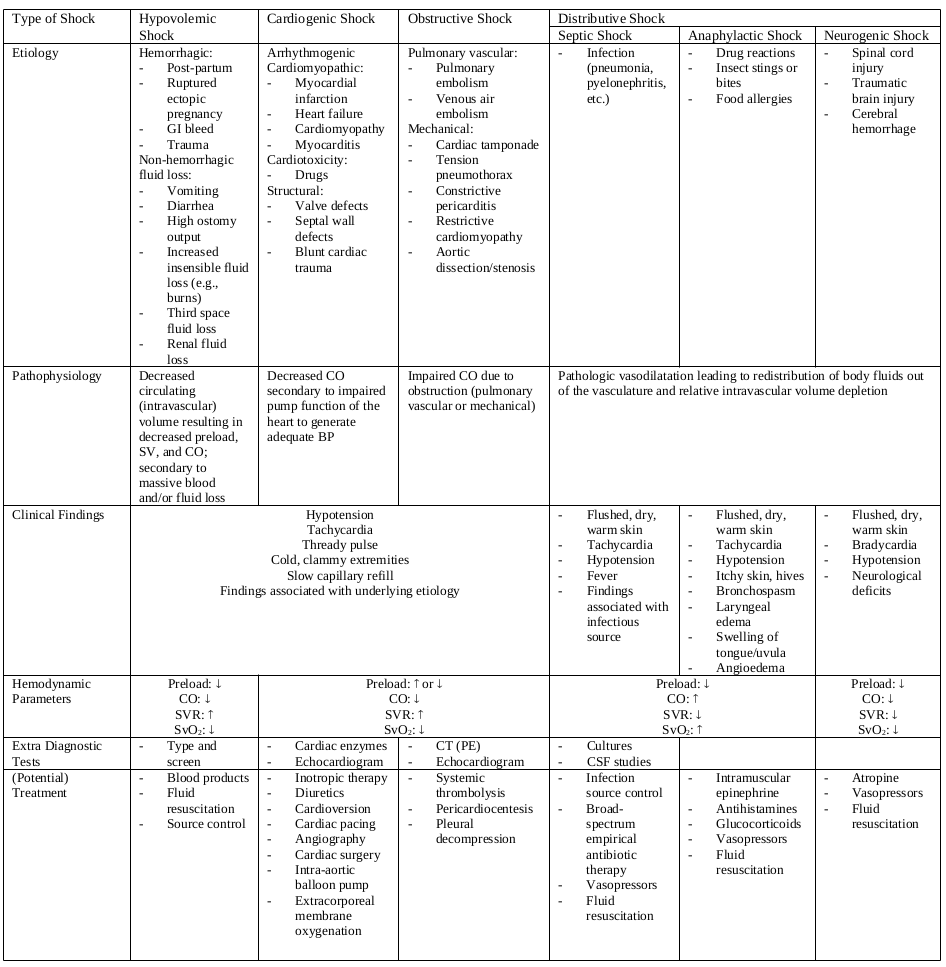
There are many different etiologies of shock, which can be broadly classified into four types of shock: hypovolemic shock (i.e., secondary to massive blood and/or fluid loss); cardiogenic shock (i.e., impaired cardiac pump function, arrhythmias, or structural defect); obstructive shock (i.e., impaired cardiac output due to obstruction); and distributive shock (i.e., pathologic vasodilatation resulting in redistribution of body fluids out of the vasculature, which can be further divided into septic, anaphylactic, and neurogenic shock) (2, 3).
The diagnosis of shock is clinical, frequently manifested by hypotension and tachycardia, as well as the findings specific to the type of shock. While some patients present with a readily identifiable etiology of shock (e.g., bleeding after trauma), other cases of shock present undifferentiated. Nevertheless, early recognition and empiric treatment are key, as shock is associated with a very high mortality rate (2, 3).
General Overview
The initial approach to shock is generally comprised of a primary survey (rapid assessment of the airway, breathing, and circulation), followed by a focused history and physical examination. A means to monitor vital signs (telemetry, blood pressure, pulse oximetry) and intravenous access with large-bore IVs should be established early on. The suspected etiology and differential diagnosis then guide further diagnostic testing; however, there is no isolated test that is specific or sensitive for shock. Studies should also be performed to determine the presence of end-organ dysfunction, which may also serve to assess response to therapy. Management of shock entails circulatory support and treatment of the underlying cause (2, 3). The individual components of the approach include (but are not limited to) the following:
History
Comprehensive history-taking may be difficult to conduct in cases of shock; obtaining collateral history may therefore be warranted. Patients may voice nonspecific complaints, such as lethargy and weakness; they may also respond inappropriately if they are presenting with altered mental status, a manifestation of cerebral hypoperfusion (2, 3).
Taking a history may reveal important symptoms and/or events that give insight into the development of shock. Trauma, melena, hematemesis, and vaginal bleeding are suggestive of hypovolemic shock secondary to hemorrhage; diarrhea, vomiting, and high ostomy output could indicate non-hemorrhagic hypovolemic shock. Cardiogenic shock or obstructive shock may be preceded symptomatically by chest pain, palpitations, shortness of breath, lower extremity swelling, or syncope. Anaphylactic shock may present with the sudden onset of skin rash, swelling, and shortness of breath following exposure to a known trigger. Septic shock may be associated with infectious symptoms: fever, chills, respiratory symptoms, dysuria, or abdominal/flank pain (2, 3).
Heart Rate
The heart rate (HR) may be elevated (>100 beats/minute) as a compensatory mechanism to maintain vital organ perfusion in cases of hypotension. However, patients with neurogenic shock may present with bradycardia due to decreased sympathetic tone (2). In older adults, a blunted tachycardic response may occur due to myocardium that is stiffened and less sensitive to catecholamines; a threshold HR of 90 may therefore define tachycardia in this population (4).
Blood Pressure
Hypotension is defined by a systolic blood pressure (BP) <90mm Hg and/or diastolic BP <60 mm Hg. Although it is commonly associated with states of shock, hypotension and tachycardia may not be present in the early stages (3, 5). A mean arterial pressure (MAP) of 60-65mm Hg is generally recognized as the minimum pressure for adequate organ perfusion (5). In adults above the age of 65, a systolic BP of less than 110mm Hg is correlated with increased mortality and considered a better benchmark to account for declining physiologic capacity, especially in the setting of trauma (4, 6).
Physical Examination
The jugular venous pressure (JVP), which reflects the patient’s fluid status and cardiac function, should be assessed visually (2, 3, 7). Signs of an elevated JVP (jugular venous distension, Kussmaul sign, hepatojugular reflex) can suggest cardiogenic and obstructive causes of shock. Murmurs, arrhythmias, and dependent edema may also accompany cardiogenic shock (2, 3). Tachypnea is frequently present, which can be related to lactic acidosis (in the context of anaerobic metabolism) or the primary insult (e.g., pulmonary embolism, pneumonia, pneumothorax, heart failure, etc.) (2, 3). The extremities may be cool to touch with thready pulses and a slow capillary refill, reflecting vasoconstriction and hypoperfusion. Conversely, the skin may be warm if there is abnormal dilatation in the early stages of distributive shock (3). It is also important to identify potential sources of hemorrhage or fluid loss. A rectal examination may be indicated to rule out melena or hematochezia. Skin integrity should be verified should there be suspicion of a burn injury (2, 3).
Hemodynamic Parameters
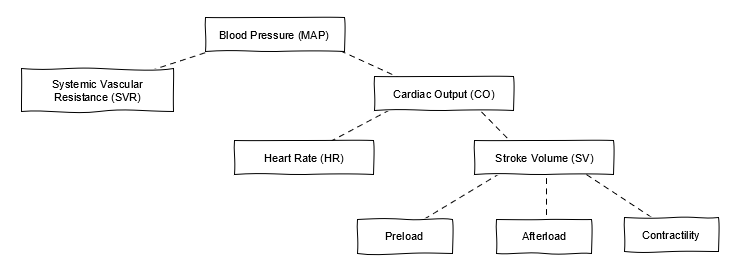
Hemodynamic parameters underlining cardiac physiology (Figure 1) may be used to characterize shock (2, 3). Preload, referring to the extent of stretch of the heart muscle fibres before the onset of systole, increases with venous constriction and increased circulating blood volume. Preload is therefore decreased with hypovolemic and distributive shock; however, it may be increased in cases of cardiogenic and obstructive shock (2, 8). Cardiac output (CO) is a measure of the blood volume (in litres) ejected from the heart in one minute. It is dependent on the stroke volume (SV) and HR. CO is increased in septic and anaphylactic shock (to maintain blood pressure), but decreased in cardiogenic, obstructive, hypovolemic, and neurogenic shock (2, 8). Systemic vascular resistance (SVR) and afterload are increased in all forms of shock except distributive shock, where there is pathologic vasodilatation (2, 3).
Mixed venous oxygen saturation (SvO2) denotes the percentage of oxygen bound to hemoglobin sampled from the right heart (i.e., the oxygen saturation of the blood from the superior and inferior vena cava as well as the coronary sinus), reflecting the body’s total oxygen consumption (2). The reference range is 65-70% (9). A decreased SvO2 reflects increased oxygen needs (e.g., due to fever, exercise, or seizures), or increased tissue extraction due to decreased oxygen delivery or availability (9). SvO2 is decreased in hypovolemic, cardiogenic, obstructive, and neurogenic shock, but may be increased in septic and anaphylactic shock (2). In the latter cases, it is proposed that high SvO2 reflecting low oxygen consumption at the tissue level may be associated with mitochondrial and microvascular dysfunction (10).
Additional Assays
Bedside Ultrasonography: (i.e., FAST examination) can narrow the differential diagnosis of shock by ruling in/out: intra-peritoneal free fluid/hemorrhage, abdominal aortic aneurysm, pneumothorax, hemothorax, cardiac tamponade, as well as assessing global cardiac function and intravascular status (3, 11).
Arterial Blood Gas Analysis: Lactic acidosis is the result of elevated serum lactate from the anaerobic metabolism in underperfused organs. The acidosis can lead to altered mental status as well as tachypnea (2).
Clotting Parameters: DIC, characterized by thrombosis, hemorrhage, and consumption of platelets and clotting factors caused by systemic activation of the clotting cascade, can develop in cases of trauma, shock, and sepsis due to their associated proinflammatory states. Typical findings include thrombocytopenia, prolonged PT and PTT, decreased fibrinogen levels, and elevated levels of fibrinogen degradation products (e.g., D-dimer) (2, 12).
Liver/Renal Function Tests: Increased urea and creatinine suggest acute renal failure as a result of kidney hypoperfusion; similarly, hyperbilirubinemia and elevated AST/ALT can indicate acute liver failure (2).
Urine Output: The patient may become oliguric, another sign of acute renal failure. This can be measured by placing a urine catheter in the bladder (2).
Beyond The Initial Approach
Table 1 summarizes the various presentations of shock, categorized by type and possible underlying etiologies, as well as their associated findings and potential treatment options.
Intravenous Fluids
Intravenous fluids are first-line agents in the management of shock to increase BP and consequently, improve organ perfusion. They are generally administered until there is an adequate BP and perfusion response, until there is evidence of harm (e.g., pulmonary edema and intra-abdominal hypertension), or when the anticipated hemodynamic response is not achieved, warranting further hemodynamic support (e.g., vasopressors).
The total volume in fluid resuscitation varies; while septic shock and hemorrhagic shock can require volumes (sometimes upward) of 2 to 5L, obstructive shock and cardiogenic shock may necessitate relatively smaller volumes, up to 1L. Although there is no one ideal choice of fluid, commonly used fluids include crystalloids (e.g., Ringer’s lactate and normal saline), as well as blood products in the setting of hemorrhagic shock (13).
Pressors in the Intensive Care Unit
Vasopressors and inotropes are an additional form of hemodynamic support used in the management of shock. They are medications that are administered intravenously, often in a continuous infusion to allow for immediate titration. Vasopressors increase vasoconstriction, resulting in increased SVR; inotropes increase cardiac contractility, which increases CO. SVR and CO in turn comprise MAP (Figure 1). A MAP of 60-65mm Hg is recognized as a reasonable target for adequate organ perfusion (5).
The most common catecholamines are phenylephrine, norepinephrine, and epinephrine, which have varying effects on alpha- and beta-adrenergic receptors. Alpha receptors induce peripheral vasoconstriction that increases SVR; beta-1 receptors have chronotropic and inotropic effects on the heart, to increase HR and contractility, respectively. Phenylephrine is a pure alpha-1 agonist that increases SVR and BP; however, it can cause reflex bradycardia. Norepinephrine and epinephrine both have alpha-1 and beta activity (to different degrees), and so they increase SVR, HR, CO, and BP (5).
Vasopressin is a peptide hormone that acts on V-1 and V-2 receptors to contract the smooth muscle of vessel walls and to increase reabsorption of water by the kidneys, respectively; this increases SVR and BP (5, 14). Dopamine is a precursor of norepinephrine and epinephrine that alters renal blood flow, SVR, HR, contractility, and CO. It acts on dopaminergic receptors as well as alpha- and beta-adrenergic receptors, and its effects vary in a dose-dependent fashion (5). Dobutamine, primarily acting on beta-1 receptors, increases contractility and CO with minimal effects on BP (5). Milrinone is a phosphodiesterase inhibitor that increases levels of cyclic AMP, resulting in cardiac stimulation (increasing CO) and vasodilatation of peripheral vessels (decreasing BP) (5).
References
- USMLE Step 1: Diagnose a patient in shock. American Medical Association. 2021. Available from: https://www.ama-assn.org/residents-students/usmle/usmle-step-1-diagnose-patient-shock
- Shock. AMBOSS. 2021. Available from: https://www.amboss.com/us/knowledge/Shock
- Sandefur B. Approach to Shock. Saem.org. 2019. Available from: https://www.saem.org/cdem/education/online-education/m3-curriculum/group-stabilization-of-the-acutely-ill-patient/approach-to-shock
- Colwell C, Moreira M, Grayzel J. Geriatric trauma: Initial evaluation and management. In: UpToDate. Waltham, MA: UpToDate; 2021.
- VanValkinburgh D, Kerndt C, Hashmi M. Inotropes And Vasopressors. Ncbi.nlm.nih.gov. 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482411/
- Southern A, Lopez R, Jwayyed S. Geriatric Trauma. Ncbi.nlm.nih.gov. 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK442020/
- Cardiovascular examination. Amboss.com. 2021. Available from: https://www.amboss.com/us/knowledge/Cardiovascular_examination
- Cardiac physiology. Amboss.com. 2021. Available from: https://www.amboss.com/us/knowledge/Cardiac_physiology
- Arterial blood gas analysis. Amboss.com. 2021. Available from: https://www.amboss.com/us/knowledge/Arterial_blood_gas_analysis
- Wittayachamnankul B, Apaijai N, Sutham K, Chenthanakij B, Liwsrisakun C, Jaiwongkam T et al. High central venous oxygen saturation is associated with mitochondrial dysfunction in septic shock: A prospective observational study. Journal of Cellular and Molecular Medicine. 2020;24(11):6485-6494.
- Whitson M, Mayo P. Ultrasonography in the emergency department. Critical Care. 2016;20(1).
- Levi M, Sivapalaratnam S. Disseminated intravascular coagulation: an update on pathogenesis and diagnosis. Expert Review of Hematology. 2018;11(8):663-672.
- Gaieski D, Mikkelsen M, Parsons P, Hockberger R, Finlay G. Evaluation of and initial approach to the adult patient with undifferentiated hypotension and shock. In: UpToDate. Waltham, MA: UpToDate; 2021.
- Morris M, Todres I, Schleien C. Cardiopulmonary Resuscitation. A Practice of Anesthesia for Infants and Children. 2009;:833-845.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.