Original Research
Sonoist: An Innovative Peer Ultrasound Learning Initiative on Canadian Teaching Hospital Wards
Laura Yan1, Kacper Niburski1, Linda Snell2,3
Published online: September 6, 2021
1Faculty of Medicine, McGill University
2Institute of Health Sciences Education, McGill University
3Division of General Internal Medicine, McGill University Health Center
Corresponding Author: Laura Yan, email laura.yan@mail.mcgill.ca
DOI: 10.26443/mjm.v20i2.856
Abstract
Background: Students usually learn point-of-care ultrasound (PoCUS) on standardized patients, thus lacking opportunities to correlate their ultrasound findings with clinical abnormalities. Sonoist is a student-led initiative aimed at improving ultrasound training with peer-teaching and real patients. We describe here a pilot project of Sonoist, its implementation and evaluation.
Methods: Sonoist was developed by Independent-Practitioner certified medical students who teach their peers how to scan patients with abnormal clinical findings, then correlate their ultrasound findings with the physical examination. From May 2019 to February 2020, seven sessions were held, with a sessional average of 3 participants and 3 patients scanned. We collected survey data on ultrasound knowledge, participants’ perceived self-improvement, and general comments. Results were grouped by prior ultrasound training (novice n=8, experienced n=12) and year of study (1-4).
Results: 20/23 completed the survey. An increase in ultrasound skill was perceived by all of novices and 67% of experienced learners. Knowledge about clinical indications for PoCUS improved in 80% of novice and 81% of experienced students; sonographic knowledge improved in 69% of novices and 81% of experienced learners. All novices and 92% of experienced learners reported that learning ultrasound was useful for correlating with physical exam and clinical diagnosis. All novices and 83% of experienced students preferred peer-to-peer teaching.
Conclusion: Peer-to-peer PoCUS teaching improved medical students’ sonographic and clinical knowledge and was perceived as useful by students. A combination of early clinical exposure and a less stressful environment from peer teaching may contribute to these results.
Tags: PoCUS, Medical education, Ultrasound, Peer teaching
Introduction
Point-of-Care Ultrasound (PoCUS) is a preferred bedside imaging method in many clinical situations. It is quick to perform, easily accessible, non-invasive, and without radiation exposure. As PoCUS is used in an increasing number of medical specialties, its incorporation into medical schools' curricula is growing.
One barrier to faculty teaching is a lack of staff who have expertise in PoCUS and time to do additional teaching outside of regular clinical duties. (1) Peer teaching, the process of using experienced students as teachers for their peers or near peers, can address this gap. Peer-teachers and their students share similar experiences and language, and have similar social roles, which promotes comfort and decreases stress. Yu et al. have shown that peer-teaching for PoCUS in undergraduate medical programs is comparable to conventional staff-teaching. (2)
Currently, undergraduate bedside ultrasound curricula focus on practicing scans with standardized patients. Scanning healthy models provides technical skills but leaves trainees with a lack of exposure to actual abnormalities and little knowledge about clinical indications to perform the scans. In addition, learning in a non-clinical setting does not encompass workplace learning, whereas interactions with patients provide informal feedback cues that allow for ongoing improvement. (3)
Sonoist is a near-peer ultrasound innovation run by medical students addressing the lack of clinical exposure in current ultrasound curricula. During Sonoist sessions, medical students scan in-patients with ultrasound-detectable findings while being taught by their Independent-Practitioner (IP) certified peers. Learners have the opportunity to correlate their ultrasound pathologies with patients’ presenting symptoms, medical history, and physical exam findings.
Given the need for appropriate ultrasound training, the effectiveness of peer teaching, and the lack of clinical and pathological exposure in current PoCUS curriculum, we hypothesize that introducing programs like Sonoist early in clinical training will increase ultrasound knowledge, skill, and understanding of pathological findings. The present study describes a pilot of the Sonoist initiative, its implementation, and evaluation.
Methods
Participants
McGill University medical students from first to fourth (final) year participated. From the students who signed up, 3-4 were selected as participants for each session on a first-come first-serve basis; this maximized scanning time while considering patient comfort. Those who signed up for multiple sessions but were not previously selected were given priority. Learners were asked to prepare by reviewing introductory video resources found on the Sonoist website (https://www.sonoist.com/) that explain the basics of each scan.
Setting
The sessions took place in university-affiliated teaching hospitals’ internal medicine wards or coronary care units (CCU), each equipped with a portable ultrasound machine. The attending physicians or senior residents on service were contacted for permission; they also offered a list of patients with potential ultrasound detectable abnormalities. The instructors met each patient prior to being scanned to obtain consent. All patients agreed to participate and were aware of the educational nature of the session.
Implementation of Sonoist
The Sonoist initiative was created by IP-certified medical students. IP is a certification provided by the Canadian Point of Care Ultrasound Society to perform, document, and teach point of care ultrasound across Canada. From May 2019 to February 2020, seven peer-taught ultrasound sessions were held, lasting 2 hours each. Because of the in-person and hands-on nature of the sessions, they had to be paused since the start of the COVID-19 pandemic. Scans taught included eFAST (free fluid), intrauterine pregnancy, lung and pneumothorax, gallbladder, subxiphoid view of the heart and advanced cardiac views. Learners were asked to prepare for each session by reviewing scans found on the Sonoist website.
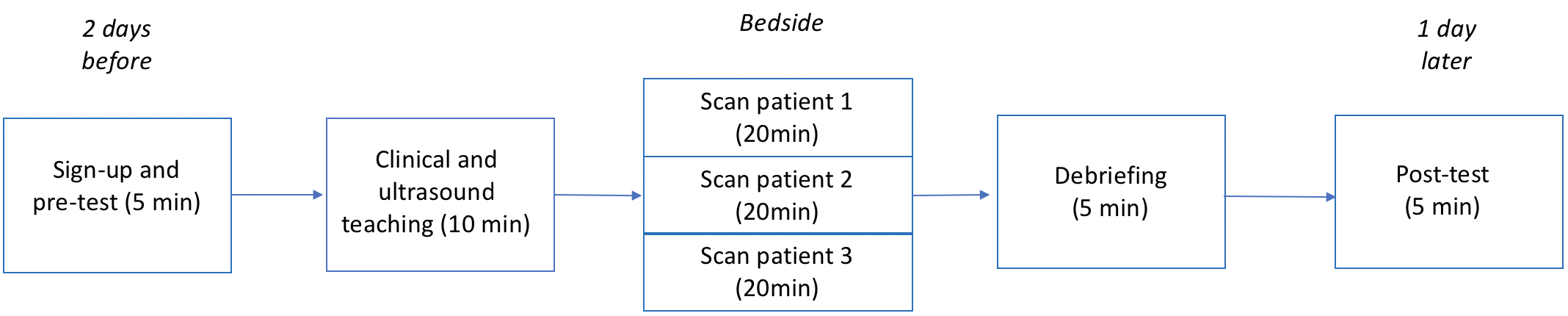
IP instructors and student participants reviewed the scans again together prior to the session (Figure 1). The group then went to the bedside and elicited a brief history. A focused physical exam was performed. Each student then practiced the indicated scan for each patient. Finally, the group debriefed by discussing the differential diagnosis, emphasizing how bedside ultrasound guided their thought process.
Program Evaluation
Pre- and post-online Google surveys collected data on the participants’ ultrasound and clinical knowledge, subjective and objective improvement, and feedback about the sessions (Table 1). The survey was adapted from other similar near-peer evaluations. (4) Questions assessed both clinical knowledge, such as indications to use PoCUS, and technical ultrasound knowledge, such as specific ultrasound findings related to a pathology. Results were de-identified and grouped by level of ultrasound training. The survey results were analyzed with descriptive statistics and two-tailed T-tests were used to determine statistical significance.
| Table 1: Pre- and post-intervention survey sent to participants | In Pre-test Survey | In Post-test Survey | Scale |
| Demographics | |||
| What is your level of ultrasound? | x | x | 1-5 |
| What is your year of study? | x | x | Free text |
| Subjective assessment | |||
| Did your technique of ultrasound improve? | x | 1-5 | |
| Was PoCUS useful to incorporate in the physical exam? | x | 1-5 | |
| Was seeing PoCUS-detectable pathologies useful in your clinical diagnosis? | x | 1-5 | |
| Was PoCUS useful clinically? | x | 1-5 | |
| Was peer-teaching helpful? | x | 1-5 | |
| Would you prefer peer-to-peer teaching or staff teaching sessions? | x | Peer vs. staff | |
| Will you advocate, or wish to use, PoCUS for your future exams? | x | 1-5 | |
| Did PoCUS help narrow your differential? | x | 1-5 | |
| Objective assessment | |||
Sonographic knowledge:
|
x | x | Multiple choice |
Clinical indications:
|
x | x | Multiple choice |
Consent to participate in the study was obtained from each participant who was made aware that the survey results were intended for research purposes. Names were only collected for the pre-intervention survey as identification was required to sign up. After the initial data was collected, they were de-identified by removing their names. Later, surveys were sent to participants via individualized URLs in order to link it with their pre-survey. During the entire process, the data remained confidential by being only available to the student researchers and not shared with any other potential clinical evaluator. Participants were free to opt out of the survey with no repercussions.
Results
23 students participated in an ultrasound session, of whom 87% (20/23) completed both a pre-test and a post-test survey. The majority were either in their second (9/20) or third (8/20) year of study. 12/20 participants had some experience, defined as previous sessions in ultrasound, and these were mostly in third year. 40% of participants were beginners, most of them being second year students with no formal training in ultrasound. Most attendees (20/23) were present for a single Sonoist session.
Subjective Skill Improvement
In response to the question “did your ultrasound technique improve,” all eight beginners reported subjective improvement, whereas 8/12 experienced participants did. Following the session, novices reported that they were much improved (4.6/5), whereas the experienced group described moderate improvement (3.8/5).
Analyzing by year yielded similar results. Students with the most experience, third years, stated subjective moderate average improvement (3.6 of 5), with only half stating they improved at all. All preclinical students, first and second years, subjectively thought they improved much more: first years subjectively improved on average 4.5 of 5 (n=2); second years improved on average 4.4 out of 5 (n=9).
Self-reported improvement pre- and post-intervention yielded similar results (Figure 2). Beginners self-reported a difference in 28% of skill, with significant results (p<0.05). Experienced users only noted an 8% increase in skill (p<0.05).
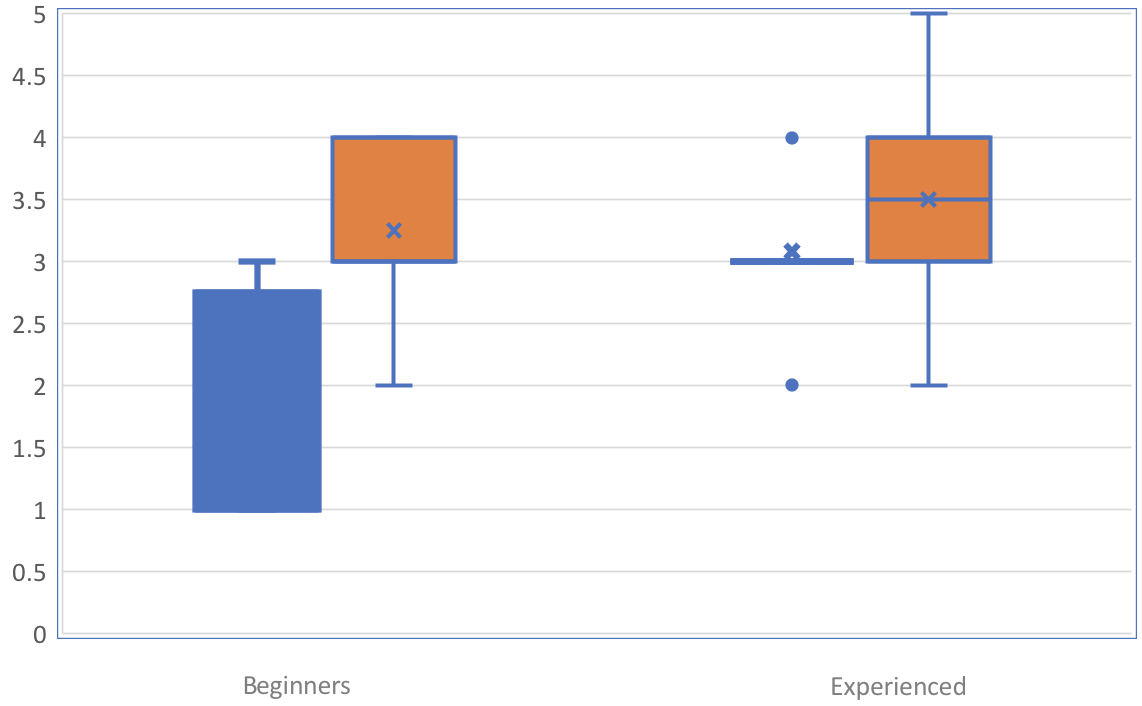
Blue is pre. Orange is post.
Students in their earlier years of training, such as those in their first year of medical school, showed the largest change of 30%, which decreased as the years went up: 16% and 13% for years 2 and 3 accordingly. No result was significant when analyzed by year.
Objective Improvement
Figure 3 shows the change in both clinical and ultrasonographic knowledge. When assessing clinical knowledge, beginners showed an increase of 31% and 44% in clinical indications and sonographic knowledge respectively. Experienced users showed an increase in 25% and 33% in clinical indications and sonographic knowledge.
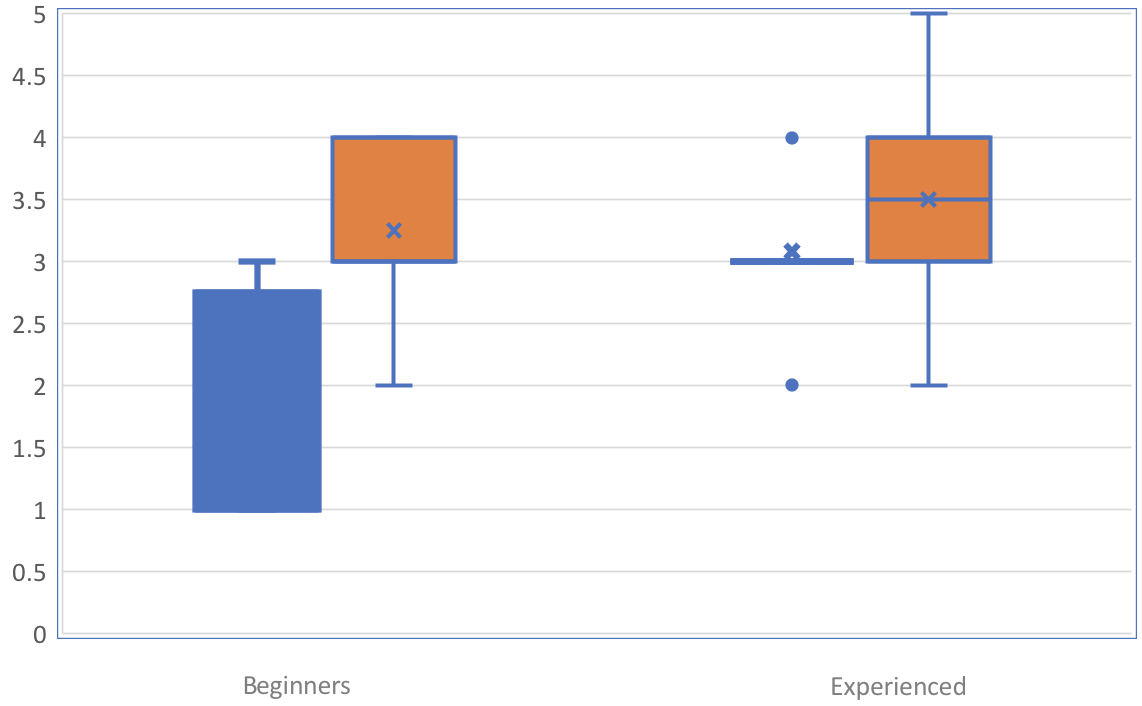
Total of 20 surveyed participants at Canadian hospital wards over 7 sessions. Blue is pre. Orange is post.
First year students showed a 50% increase in clinical indication and 50% in technical sonographic knowledge; second years showed a 55% increase in clinical indication and 61% in technical ultrasound knowledge; and third years showed a 25% increase in clinical indication and 37% in actual ultrasound knowledge.
Physical Exam with PoCUS
All beginners reported that the use of ultrasound was better than physical exam alone, with an average score of 4.8 of 5 when answering the question “was PoCUS useful to incorporate in the physical exam?”. 92% of experienced users stated that it was useful, with a score of 4.4 of 5. With this, all beginners stated that there was utility in narrowing the differential diagnosis using ultrasound, especially for pathognomonic findings, with a score of 4.9 of 5. All experienced users stated similarly, with a score of 4.8 of 5.
All participants, except two students from second year, suggested that ultrasound was a necessary adjunct for the physical exam. Only one (1/9) second year stated it was not necessarily useful, though the average usefulness for clinical use and narrowing the differential was highest in this group at 4.9 of 5.
Utility and Peer Teaching
All users (20/20) reported that the sessions were useful and agreed that ultrasound would likely be used in the future, as well as advocate for its use in clinical scenarios where appropriate.
With regards to peer-to-peer teaching, all novices, as well as those in first and second year, preferred student-led sessions, whereas 83% (10/12) of experienced users did. Of those in their third year, 8/9 preferred student sessions and 0/1 in fourth year did.
Discussion
We report the first use of combining teaching through patients with real clinical findings and peer-to-peer ultrasound as a means to increase ultrasonographic and clinical knowledge. An increase in ultrasound knowledge and subjective skill were observed in both beginners and experienced learners, though most significantly in self-identified beginners. The positive effects of ultrasound noted in the literature, such as an increase in clinical indication and pathological identification, were similarly noted. Moreover, learners of all levels stated their preference for peer-to-peer teaching over staff teaching.
The benefits of peer teaching are well known: it provides a comfortable learning environment for students, allows peer-instructors to consolidate their knowledge through teaching and use less medical education resources to achieve comparable results. (5, 6) This is the first published study, however, to show its use on real patients with positive ultrasound findings. Although benefits were observed in all groups, they differed in their perception of gains. For example, experienced users perceived that they improved much less than their objective scores suggested. Beginners, however, believed they improved more proportionally to their objective scores. The latter could be explained by learners equipped with less knowledge having lower expectations of their improvement compared to more advanced learners. Providing early exposure in a low-stress environment, therefore, may be key in ensuring greater perceived benefits and self-confidence for students in ultrasound.
Similarly, preclinical students in their first or second year of study showed the largest subjective perceived improvement with a mirrored increase in their quantitative measures. This suggests the presence of a steeper learning curve in the initial phase of ultrasound education. Such a trend is not uncommon in medical education, where it has often been noted that pre-clinical exposure maximizes learning for beginning medical practitioners. (7)
The increased clinical and ultrasound knowledge might further be explained by workplace learning concepts, where learners feel they are included in actual hospital work. (3) Many transitional clerkship curricula attempt to mirror this learning by exposing pre-clerkship students to authentic clinical settings. (7) As more schools foster early clinical exposure, it is likely ultrasound curricula will need to incorporate projects like Sonoist to mirror actual sonographic work.
There are limitations in this study. Because the project was brought to a halt since the start of the COVID-19 pandemic, it was conducted only at two sites with a few patients and pathologies; however, we feel that the patients’ pathologies generally represent what a medical student might see at a typical teaching hospital.
Additionally, though the majority of the feedback received from each session was positive, there are key questions remaining. What are other contexts in which peer-teaching is preferred over staff teaching? What would be the effect of using peer-instructors with less training? Previous PoCUS initiatives noted that different levels of effective instructorship relied on their comfort with both the technical and clinical aspects of ultrasound. (3) Novice instructors may require further training to ensure excellence in teaching, and to properly identify clinical findings. Further work will go into creating a skill-based assessment of students and instructors who are being observed and graded undertaking POCUS.
Importantly, most participants preferred peer clinical teaching. Possible reasons include low stress roles without significant responsibility, comfortable learning environments, and the ability to have first on-hand exposure. Thus, Sonoist is a promising initiative that addresses the need for qualified faculty by putting students at the forefront of innovation. Such student exposure and teaching may be increasingly necessary, with ultrasound seen as a future “fifth pillar of physical examination”. (8)
Peer-to-peer teaching like Sonoist improves sonographic, clinical knowledge of both experienced and beginner PoCUS practitioners, increases perceived benefit and advocacy for PoCUS, and is preferred over other staff teaching in this specific context. It is a helpful tool that requires further investigation on learning strategies and styles but offers a promising future.
References
- Acuña J, Rubin M, Hahn B, Das D, Kapoor M, Adhikari S, Greenstein J. Point-of-Care Ultrasound in United States Pediatric Emergency Medicine Fellowship Programs: The Current State of Practice and Training. Pediatr Emerg Care. 2020 Feb 28. doi: 10.1097/PEC.0000000000001955.
- Yu TC, Wilson NC, Singh PP, Lemanu DP, Hawken SJ, Hill AG. Medical students-as-teachers: a systematic review of peer-assisted teaching during medical school. Adv Med Educ Pract. 2011 Jun 23;2:157-72. doi: 10.2147/AMEP.S14383.
- Dornan T, Boshuizen H, King N, Scherpbier A. Experience-based learning: a model linking the processes and outcomes of medical students' workplace learning. Med Educ. 2007 Jan;41(1):84-91. doi: 10.1111/j.1365-2929.2006.02652.x.
- Smith, C.J., Matthias, T., Beam, E. et al. Building a bigger tent in point-of-care ultrasound education: a mixed-methods evaluation of interprofessional, near-peer teaching of internal medicine residents by sonography students. BMC Med Educ 18, 321 (2018). https://doi.org/10.1186/s12909-018-1437-2.
- Allikmets S, Vink JP. The benefits of peer-led teaching in medical education. Adv Med Educ Pract. 2016;7:329–30. doi: 10.2147/AMEP.S107776.
- Dickerson J, Paul K, Vila P, Whiticar R. The role for peer-assisted ultrasound teaching in medical school. Clin Teach. 2017 Jun;14(3):170-174. doi: 10.1111/tct.12541. Epub 2016 Jun 27.
- Koens F, Mann KV, Custers EJ, Ten Cate OT. Analysing the concept of context in medical education. Med Educ. 2005;39:1243–1249. doi: 10.1111/j.1365-2929.2005.02338.x.
- Narula J. Chandrashekhar Y, Braunwald E. Time to add a fifth pillar to bedside physical examination: Inspection, palpation, percussion, auscultation, and insonation. JAMA Cardiol. 2018;3(4):346-350. doi:10.1001/jamacardio.2018.0001.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.