Approach to
Hyponatremia
Kaylie Schachter1
Published online: 31 May 2021
1Faculty of Medicine, McGill University, Montreal, Quebec, Canada
Corresponding Author: Kaylie Schachter, email kaylie.schachter@mail.mcgill.ca
DOI: 10.26443/mjm.v19i1.833
Abstract
Hyponatremia is a common laboratory finding in numerous patients. It is defined as a serum sodium concentration <135 mmol/L and represents an excess of water in the extracellular compartment. The severity of this electrolyte abnormality ranges from asymptomatic to seizures, coma and death as a consequence of cerebral swelling. There are multiple medical conditions, medications and disease states that can cause hyponatremia. This article summarizes the important pathophysiological pathways involved in the development of hyponatremia, describes an approach to common causes and reviews the initial steps in management.
Tags: Hyponatremia, Syndrome of Inappropriate Anti-Diuretic Hormone, Vaptans
Question
A 72-year-old man, previously well, presents to the emergency department with a 5-day history of fever, productive cough and dyspnea. His past medical history includes type 2 diabetes mellitus, gastroesophageal reflux disease and dyslipidemia. His medications include metformin, pantoprazole and atorvastatin. On physical exam, the patient appears well. He is hemodynamically stable with a temperature of 38°C. His exam is remarkable for crackles and decreased air entry in the right middle lobe. He has no pitting edema, no ascites, no jugular venous distension, and his mucous membranes are moist. His laboratory results are as follows (normal values in brackets):
- Hemoglobin 137 (125-170 g/L)
- Mean corpuscular volume 83 (80-100 fL)
- White blood count 13 x 109/L (3.5-10.5 x 109/L)
- Platelets 200 x 109/L (130-380 x 109/L)
- Absolute neutrophil count 9 x 109/L (2-7.5 x 109/L)
- Na 129 (136-146 mmol/L), K 4 (3.5-5.1 mmol/L), Cl 107 (98-107 mmol/L)
- Bicarbonate 24 (21-32 mmol/L)
- Blood urea nitrogen 7.9 (2.1-8 mmol/L), Creatinine 81 (49-93 µmol/L)
- Glucose random 6.7 (4-11 mmol/L)
- Thyroid- stimulating hormone 1.16 (0.34-5.60 mIU/L)
- AM cortisol 550 (185-624 nmol/L)
- Plasma osmolality: 273 (275-295 mmol/kg)
- Urine sodium: 50 mmol/L (elevated)
- Urine osmolality: 480 mOsm/ kg (38-1400 mOsm/kg H2O)
Given the most likely cause of this patient’s hyponatremia, what is the next step in management?
- IV infusion of 3% saline
- Vaptans
- IV infusion 0.9% saline
- Start diuretics
- Fluid restriction
Answer
E. The patient in this scenario most likely has SIADH (syndrome of inappropriate anti-diuretic hormone) secondary to his pneumonia. This is evidenced by the patient’s euvolemic hypo-osmolar hyponatremia, with a reduced plasma osmolality, concentrated urine, and elevated urine sodium. Other causes, such as hypothyroidism and adrenal insufficiency, have been ruled out with the normal laboratory values. The first step in managing SIADH is to restrict the patient’s fluid intake (E). Hypertonic saline is used in cases of severely symptomatic hyponatremia, whereas this patient has no evidence of symptoms secondary to his hyponatremia (A). Vaptans would be considered for refractory hyponatremia (B). The use of normal saline is appropriate when the patient has evidence of volume depletion, which is not the case for this patient (C). If normal saline were to be given, it would be expected that Na would decrease in the case of SIADH. Diuretics would be prescribed to a patient with congestive heart failure, which this patient is not presenting with (D).
Definition and Pathophysiology
Hyponatremia is defined as a measured serum sodium concentration less than 135 mmol/L. Hyponatremia is a pathophysiological process representing an excess of water in the extracellular compartment relative to the amount of sodium. (1)
Water exists throughout the body in two distinct compartments: intracellular and extracellular. The extracellular compartment can be subdivided into the plasma and interstitium. Water is able to move freely between the intracellular and extracellular compartments. (2)
In addition to water, there are solutes in these two compartments which contribute to the osmolality. The plasma osmolality (Posm) is one of the main factors that contributes to water regulation as it must remain constant (between 280-295 mOsm/kg) and equal to the intracellular osmolality. (2) Posm can be measured or calculated with the following equation: Posm= 2[Na+] + [glucose] + [blood urea nitrogen].
Osmoreceptors in the hypothalamus detect the plasma osmolality. If Posm >285 mOsm/kg, osmoreceptors stimulate the release of anti-diuretic hormone (ADH) from the posterior pituitary into the circulation, as well as stimulate thirst. ADH release is also stimulated in states of low effective circulating volume. (1, 2) Circulating ADH binds to receptors on the principal cells of the collecting duct in the kidneys and activates a cellular pathway which ultimately results in water reabsorption. This results in a decrease in the serum osmolality and an increase in the urine osmolality (Uosm). (2) In certain states, ADH can be released inappropriately or ectopically, meaning that ADH is released without an osmotic or hemodynamic stimulus. (3) When ADH is suppressed, water is renally excreted. (2)
Another important physiological pathway is the renin-angiotensin-aldosterone system (RAAS). This pathway is activated in states of low effective circulating volume and/or when there is reduced sodium in the renal tubules. These conditions stimulate the release of renin from the juxtaglomerular cells, which are part of the afferent arterioles. The activation of RAAS ultimately results in increased sodium reabsorption, arteriolar vasoconstriction and release of ADH from the posterior pituitary. (4) Measured urine sodium concentration (UNa) is a reflection of intravascular volume; UNa is elevated with volume expansion and reduced with volume depletion. (3)
Hyponatremia is a common laboratory finding in the inpatient and outpatient settings. (5) As a result of low sodium concentration in the extracellular fluid, water will freely move intracellularly to maintain osmotic equilibrium, resulting in cellular swelling. Hyponatremia can be classified as acute (<48 hours) or chronic (>48 hours) and by severity, as mild (130-134 mmol/L), moderate (125-129 mmol/L) and severe (<125 mmol/L). (1) When hyponatremia develops chronically (>48 hours), cells can adapt by losing cellular electrolytes and organic osmolytes (6), ultimately resulting in less cellular edema. When cells do not have time to adapt (<48 hours), cerebral swelling could ensue and result in neurological symptoms ranging from headache, nausea, and vomiting, to altered mental status, seizures, brain herniation, and coma. (2, 7)
Initial Approach
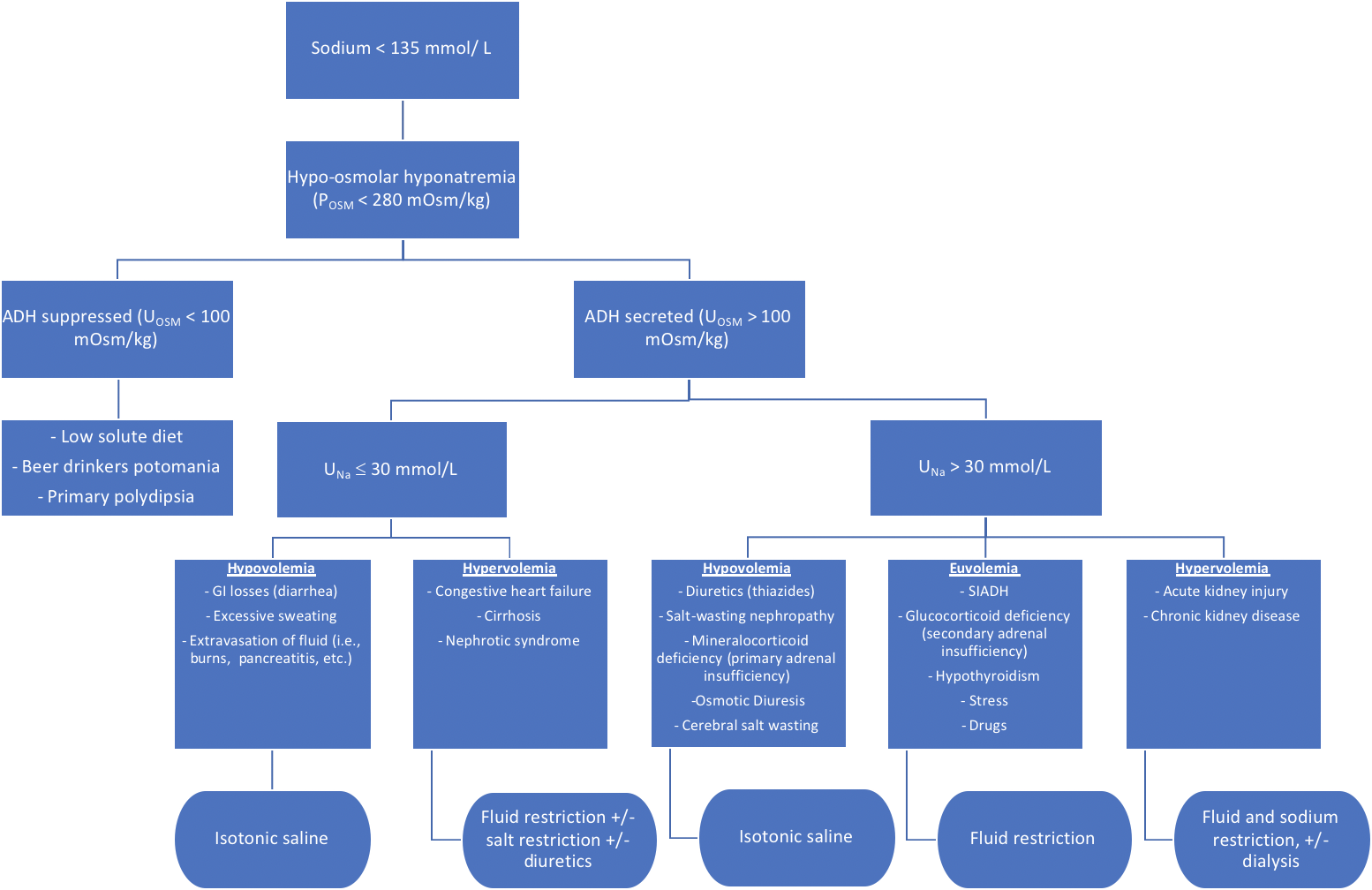
The etiology of hyponatremia includes a wide range of medications, medical conditions, and other disease states. Therefore it requires a thorough, stepwise approach to ensure the correct diagnosis is made and the most appropriate treatment can be provided.
Is this a “true” hyponatremia?
First, determine if the patient has hypo-osmolar hyponatremia, also known as “true hyponatremia.” If measured plasma osmolality is <275 mOsm/kg and the serum sodium is <135 mmol/L, then the patient has “true hyponatremia”. (1)
If a patient with hyponatremia is found to have a plasma osmolality in the normal range (280-295 mOsm/kg) or above normal range (>295 mOsm/kg), then the patient has “iso-osmolar hyponatremia” (also known as “pseudohyponatremia”) or hyper-osmolar hyponatremia, respectively. In these cases, additional osmoles are contributing to the plasma osmolality, such as glucose, lipids, or proteins. (1) Nowadays, pseudohyponatremia is less commonly seen as laboratories can correct for these additional osmoles. (8)
This article will focus on hypo-osmolar hyponatremia.
Is ADH suppressed or secreted?
ADH is suppressed (Uosm <100 mOsm/kg)
Hyponatremia can result in the context of excess water intake relative to solutes consumed. In these situations, ADH activity is absent and the kidneys excrete water to produce a maximally dilute urine (Uosm <100 mOsm/kg). (1) However, there is a maximum amount of water that can be excreted, which can result in excess water in the extracellular compartment relative to sodium. Etiologies include “tea and toast” diet, beer drinkers’ potomania, or primary polydipsia. (1) Excess water consumption is considered drinking approximately > 1L/hour. (3)
ADH is secreted (Uosm >100 mOsm/kg)
When ADH is secreted, the kidneys reabsorb water, resulting in a concentrated urine. Once known that Uosm >100 mOsm/kg, the next step is to determine the intravascular volume by assessing the urine sodium concentration.
What is the intravascular volume: UNa ≤30 mmol/L or UNa >30 mmol/L?
In states of low effective arterial blood volume, RAAS is activated and increased sodium is reabsorbed from the urine, resulting in a UNa ≤30mmol/L. (4) With normal or elevated effective circulating volume, UNa >30 mmol/L. (1)
What is the patient’s volume status?
Once UNa is known, patients must be evaluated clinically to determine their overall volume status.
Hypovolemia
Patients who are hypovolemic may have non-specific symptoms, such as fatigue, weakness, thirst, and postural dizziness. (2) On exam, they may have decreased jugular venous pressure (JVP), orthostatic tachycardia, orthostatic hypotension, dry mucous membranes, decreased skin turgor, and decreased urine output (unless on a diuretic). Their laboratory values may show an elevated creatinine, blood urea nitrogen or hematocrit. (2, 6)
In patients with UNa <30 mmol/L, hypovolemic hyponatremia can be caused by gastrointestinal fluid loss (e.g. diarrhea), excessive sweating, or extravasation of fluid (previously known as third spacing), in which the intravascular volume is depleted leading to the activation of ADH and thus free water retention. (1, 6, 9)
In patients with UNa >30 mmol/L, hypovolemic hyponatremia is often due to renal loss of sodium and water. This includes any cause of hypoaldosteronism (e.g. primary adrenal insufficiency), salt-wasting nephropathies, diuretic use (especially thiazides) and osmotic diuresis. (2)
Euvolemia
Etiologies of euvolemia with UNa >30 mmol/L include syndrome of inappropriate ADH (SIADH), hypothyroidism, and secondary adrenal insufficiency. SIADH should only be diagnosed once renal disease, hypothyroidism, adrenal insufficiency, and thiazide use have been ruled out. (1) SIADH is the most common cause of euvolemic hyponatremia, in which ADH is secreted despite normal Posm and normal circulating volume. There are many known causes of SIADH, including lung diseases (e.g. pneumonia), pain, nausea, CNS lesions, and drugs (selective serotonin reuptake inhibitors, tricyclic antidepressants, antipsychotic medications, etc.) (2, 6). Certain cancers, such as small cell lung cancer and olfactory neuroblastoma, can give rise to ectopic ADH production. (10)
Criteria for diagnosing SIADH is found in Table 1.
| Table 1: Essential criteria to diagnose syndrome of inappropriate antidiuretic hormone | Effective serum osmolality | <275 mOsm/kg |
| Urine osmolality | >100 mOsm/kg | |
| Urine sodium | >30 mmol/L (with normal salt and water intake) | |
| Clinically euvolemic | No evidence of volume overload or volume depletion (i.e., hemodynamically stable, no postural symptoms, normal JVP, normal mucous membranes, no crackles, no S3, no ascites, no edema) | |
| No other contributing illness | Rule out adrenal, thyroid, pituitary or renal insufficiency No recent use of diuretics |
|
Hypervolemia
Patients who are hypervolemic may have an elevated JVP, inspiratory crackles, S3 (third heart sound), ascites, or edema. Laboratory results may show a decreased hematocrit and serum protein. (6)
In patients with UNa <30 mmol/L, hypervolemic hyponatremia can be caused by congestive heart failure (CHF), cirrhosis, or nephrotic syndrome. Patients with these illnesses can be in states of low effective circulating volume but clinically appear hypervolemic. (1, 11)
Hypervolemic hyponatremia in the context of UNa >30 mmol/L can occur in renal failure, due to impaired free water excretion. (7)
Beyond the Initial Approach
The management of hyponatremia is based on its acuity, severity, volume status, and etiology. The approach above helps to determine the most likely diagnosis, which will then guide the most appropriate management. The main principle of treating hyponatremia is to treat the underlying cause.
Acute, severe or symptomatic hyponatremia should be managed immediately to reduce the risk of cerebral edema, seizure, and brain herniation. It should be initially treated with 3% hypertonic saline. (11) Rates of correction should not exceed 6 to 8 mmol/L per day to avoid the risk of developing osmotic demyelination syndrome, a complication that results in paraplegia, dysarthria, dysphagia, diplopia, “locked-in syndrome”, or loss of consciousness. (2, 12) Patients must be closely monitored with serial blood tests to evaluate the correction rate.
In hypovolemic hyponatremia, the effective circulating volume must be restored with an intravenous infusion of normal saline. Once intravascular volume is restored, ADH will be suppressed, resulting in renal excretion of water and rapid correction of the hyponatremia. (11) Urine output should be monitored, as an output >100 ml/hour can be a sign of correcting too rapidly. (9) Serial blood tests should be ordered to monitor the correction rate.
Euvolemic hyponatremia can be due to several underlying conditions, including low solute intake or excess fluid intake. These conditions can be addressed by increasing the patients’ solute intake or restricting fluid intake. If the hyponatremia is secondary to hypothyroidism or adrenal insufficiency, the management plan should include fluid restriction as well as treatment to address the underlying disease. (11)
SIADH, a cause of euvolemic hyponatremia, is initially managed with fluid restriction in addition to investigating and treating the underlying etiology. Increasing solute intake may be helpful in order to increase electrolyte-free fluid excretion. Vaptans, a medication that antagonizes the effects of ADH, can be added to the management plan if the above methods fail. (11)
Hypervolemic hyponatremia is generally managed with fluid restriction. When caused by CHF or cirrhosis, patients tend to respond to fluid and salt restriction. In CHF, and cautiously in cirrhosis, loop diuretics should also be started as part of the first-line management. A second-line option could include vaptans. (11)
Abbreviations: Posm= plasma osmolality
ADH= antidiuretic hormone
Uosm= urine osmolality
UNa= urine sodium
CHF= congestive heart failure
SIADH= syndrome of inappropriate antidiuretic hormone
AKI= acute kidney injury
CKD= chronic kidney disease
Adapted from
Spasovski G, Vanholder R, Allolio B, Annane D, Ball S, Bichet D, et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Intensive Care Med. 2014;40(3):320-31.
Toronto Notes 2020. 36th ed. Senevirante SMaA, editor. Toronto, Canada2020.
Sabatine MS. Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine: Wolters Kluwer Law & Business; 2016. Orange Book
Braun MM, Barstow CH, Pyzocha NJ. Diagnosis and management of sodium disorders: hyponatremia and hypernatremia. Am Fam Physician. 2015;91(5):299-307.
Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrison's Principles of Internal Medicine 19/E (Vol.1 & Vol.2): McGraw-Hill Education; 2015.
References
- Spasovski G, Vanholder R, Allolio B, Annane D, Ball S, Bichet D, et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Intensive Care Med. 2014;40(3):320-31.
- Hoorn EJ, Zietse R. Diagnosis and Treatment of Hyponatremia: Compilation of the Guidelines. J Am Soc Nephrol. 2017;28(5):1340-9.
- Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrison's Principles of Internal Medicine. 19th ed: McGraw-Hill Education; 2015.
- Sterns RH. Disorders of plasma sodium--causes, consequences, and correction. N Engl J Med. 2015;372(1):55-65.
- JH Fountain SL. Physiology, renin angiotensin system. 2017.
- Yeates KE, Singer M, Morton AR. Salt and water: a simple approach to hyponatremia. Cmaj. 2004;170(3):365-9.
- Toronto Notes 2020: Comprehensive Medical Reference and Review for the Medical Council of Canada Qualifying Exam (MCCQE) Part I and the United States Medical Licensing Exam (USMLE) Step II 36th ed: Toronto Notes for Medical Students, Incorporated; 2020.
- Mathew A KF, Franek E, Drabczyk R. Hyponatremia. McMaster Textbook of Internal Medicine. Kraków: Medycyna Praktyczna; 2019.
- Seay NW, Lehrich RW, Greenberg A. Diagnosis and Management of Disorders of Body Tonicity-Hyponatremia and Hypernatremia: Core Curriculum 2020. Am J Kidney Dis. 2020;75(2):272-86.
- Theis SR, Khandhar PB. Pseudohyponatremia. StatPearls. Treasure Island (FL): StatPearls Publishing LLC.; 2021.
- Braun MM, Barstow CH, Pyzocha NJ. Diagnosis and management of sodium disorders: hyponatremia and hypernatremia. Am Fam Physician. 2015;91(5):299-307.
- Sabatine MS. Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine: Wolters Kluwer Law & Business; 2016.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.