Approach to
Acute Lower Back Pain (LBP) in the Primary Care Setting
Philippe Moisan1
Published online: 22 May 2021
1McGill University, Montreal, QC, Canada
Corresponding Author: Philippe Moisan, email philippe.moisan@mail.mcgill.ca
DOI: 10.26443/mjm.v19i1.827
Abstract
Between 50 and 80% of adults will experience lower back pain during their life. (1) This condition is responsible for a significant portion of emergency room and primary care consultations and it creates a significant burden on the healthcare services and costs. Even if lower back pain causes a significant impact on the quality of life of the patients most causes are benign. This article presents a systematic approach to identifying the cause of lower back pain, summarizes the indications for further workup and presents current evidence for the management of this condition.
Tags: Lower back pain, Physical treatment, Pharmocology, Family medicine, Orthopedic Surgery
Question
Miss M. is a 55-year-old female who works as a cashier in a grocery story. She has hypertension, dyslipidemia and diabetes. She takes Lipitor, Metformin and Ramipril. describes herself as physically inactive. She presents to her family doctor complaining of a diffuse pain localized in her lower back. Although she is unable to put a finger on the pain, she tells you that it’s worse at the end of her workday and has been going on for the last 2 weeks. She is taking Tylenol for the pain which seems to help. She denies any incontinence, saddle anesthesia, leg weakness or numbness.
On physical examination she has no point tenderness on palpation of her back, a normal range of motion, strength of the lower extremities is 5/5 on both sides, and her sensation to light touch over dermatomes L2-S2 is normal and symmetrical. She has 2+ reflexes at her patellar and Achilles tendon bilaterally. Examination of her gait is normal and a straight leg raise reveals minor pain on the right side throughout the range of motion.
She tells you that her sister has a herniated disk. She is worried that she may have the same condition and requests an MRI.
As the family doctor, what is the next best step?
- Order an MRI to rule out neural compression or malignancy
- Prescribe two weeks of muscle relaxants and narcotics for the pain
- Give her a medical leave from work and recommend bedrest for three days.
- Reassure her that she does not need an MRI as this is likely benign and self-limited.
- Urgent referral to a neurosurgeon.
Answer
D. This is a physically inactive patient that has started a new job which requires a significant amount of standing. She does not report trauma, is not known for risk factors of pathological spine fracture, and has no history of cancer. She comes in complaining of symptoms that correspond to this new physical demand. The description of her symptoms are localized to her lower back with no radiation, and appears with fatigue at the end of the day. The physical examination is completely normal and she has no signs or symptoms of cauda equina syndrome. This case represents an uncomplicated mechanical back pain without worrisome features. This condition is common, requires no investigations and is self-limited. Reassurance is the mainstay of treatment, but physical treatment, non-steroidal anti-inflammatory medications might help the symptoms.
Initial Approach
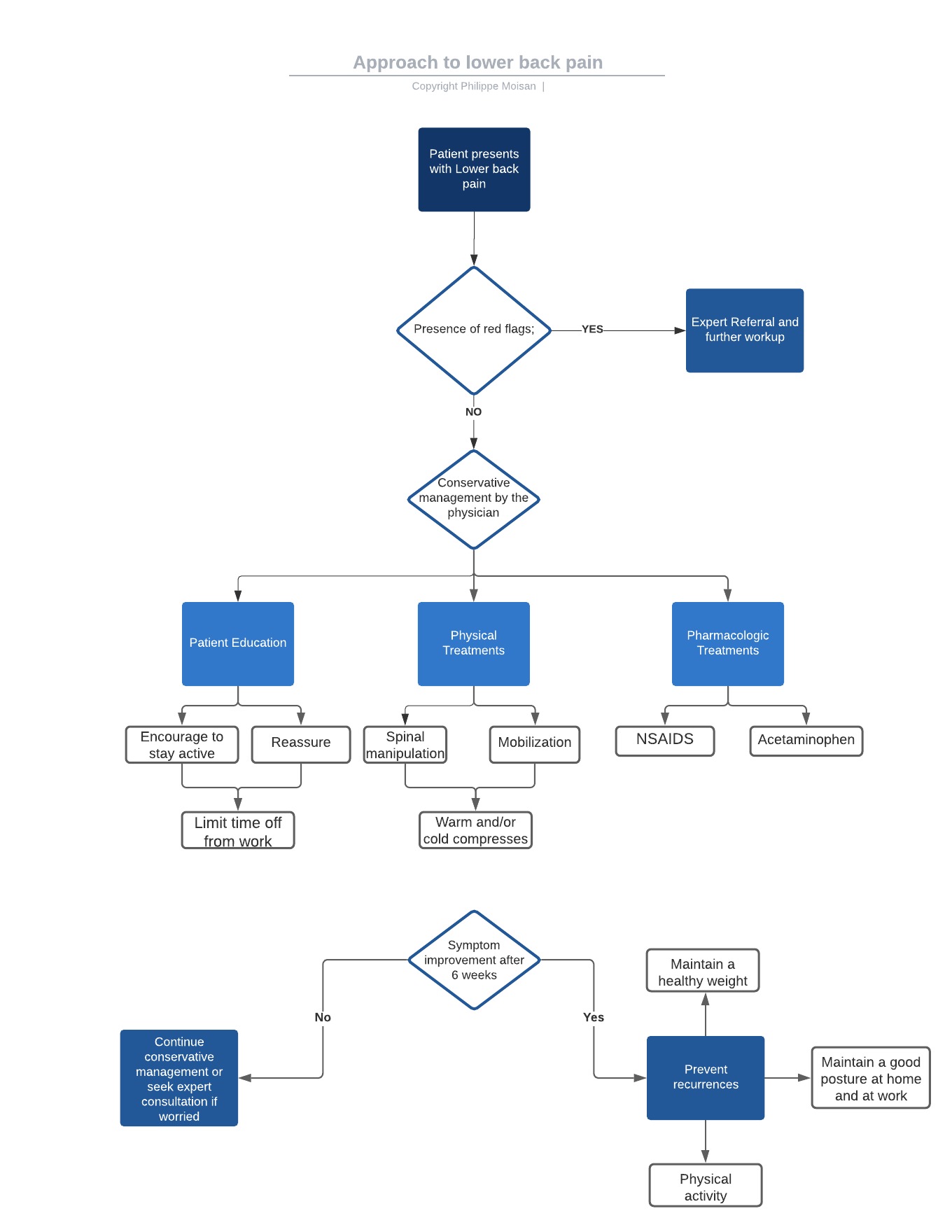
When a patient presents with lower back pain, we are interested in understanding the mechanism of injury, onset of the symptoms, location and radiation of the pain, provoking factors, associated neurologic deficits and systemic manifestations to determine whether the cause of the symptoms is worrisome or not (Fig. 1). Common causes are described later and summarized in Table 2. The next step is to provide expert referral and further workup when a serious etiology is suspected. In cases of benign causes of lower back pain, the three key components of management are described later in the text.
| Table 2: Summary of causes of lower back pain | Benign | Dangerous |
| Mechanical | Muscle strain
Degenerative back pain Sacroiliac symptoms |
Fracture (potentially) |
| Malignant | Metastasis Multiple myeloma |
|
| Neurogenic | Radicular back pain (sciatica) | Cauda equina syndrome |
Red flags of lower back pain
While questioning the patient, the clinician must keep in mind that their main goal is to differentiate benign from potentially dangerous and devastating causes of lower back pain. Cauda equina syndrome is the most time-sensitive and potentially catastrophic cause of lower back pain. To assess the risk of the patient having a serious cause for their symptoms, it is imperative to look for red flags (Table 1).
| Table 1: Red flags of lower back pain | Trauma | |
| History of cancer | ||
| Systemic symptoms (weight loss, fever…) | ||
| Urinary or fecal incontinence | ||
| Steroid use | ||
| Progressive neurologic deficit | ||
| Saddle anesthesia | ||
| Immunosuppression | ||
| IV drug use | ||
Physical Examination
A pertinent physical examination includes the inspection of the back for deformities, bruises or skin changes. Palpation of the spine and paravertebral soft tissues can allow the clinician to elicit a focal area of tenderness which might help in differentiating a skeletal from a muscular etiology. Examination of the range of motion and gait will give the examiner an estimation of the functional deficit and may hint to inflammatory causes, infectious causes, or neurologic impairment. A quick distal neurologic examination is essential and should include testing light touch sensation, strength of the L2 to S2 myotomes, and testing the reflexes of the patellar and Achilles tendons.
Common and less common causes of lower back pain
Mechanical causes
Muscle strain: This is the most common cause of back pain. It often appears in the context of rapid movement or physical activity. The pain is usually acute and associated with reproducible tenderness on paravertebral palpation. It is characterized by stiffness and difficulty bending the spine. It is self-resolving and improves with rest, ice, and analgesia.
Fracture: Vertebral compression fractures account for 4% of patients that present to a primary care setting complaining of back pain. (1) In the context of high energy trauma and is likely to be pathological when no trauma is involved. The index of suspicion of fractures should be high in patients with cancer and osteoporosis. Spine fractures are potentially unstable and might lead to neural compromise if not treated appropriately. Fractures require consultation with a spine surgeon.
Degenerative back pain: It is caused by facet degeneration. This cause is more common in older adults and is worse with physical activity such as standing for long periods of time or lifting objects. It is not associated with trauma. Patients will describe it as dull, worse at the end of the day, and worsened by exertion.
Sacroiliac symptoms: The pain is located in the lower back overlying the sacroiliac joint. It is often bilateral, worse when standing still and with activity.
Malignancy
The clinician should have a high index of suspicion in patients with a history of cancer. The patient often describes an insidious onset and systemic symptoms such as weight loss, anorexia, and night pain. These patients are at high risk for complications and pathologic fractures. When cancer is suspected as the cause of back pain, an expert consultation is warranted.
Infectious
Infectious causes of back pain are often associated with fever and systemic symptoms. It is common in a patient who recently underwent a spine surgery, is an IV drug user, or has had a recent bacteremia. An epidural abscess is an urgent infectious cause that requires timely diagnosis and immediate treatment with intravenous antibiotics as well as a surgical consultation for possible drainage. Patients coming from a tuberculosis endemic region of the world that present with multi-level back pain should raise the suspicion of tuberculous spondylitis.
Neurogenic
Radicular pain: It is a condition more common in older adults and is associated with unilateral leg pain in a dermatomal distribution. It is called sciatica when the radiating pain follows the course of the sciatic nerve (posterior or lateral leg extending to the foot or ankle) due to irritation of the L5-S1 spinal roots. The patient might have a positive straight leg raise test and their symptoms are usually not acute. Symptomatic disk herniations or spinal stenosis account for 3-4% of cases of back pain seen in primary care. (1)
Cauda Equina syndrome: This syndrome is caused by the neural compression of the cauda equina. This is a surgical emergency. Worrisome findings on history or physical exam such as bilateral leg pain, lower extremity weakness, saddle anesthesia, bowel or bladder symptoms warrant further worker and urgent neurosurgical or orthopedic surgery consultation. Cauda equina syndrome is most commonly due to disk herniation, ankylosing spondylitis, lumbar puncture, trauma or malignancy. (2)
Working up lower back pain
After having considered the demographics of the patient, taking a history and conducting a focused physical examination, the clinician will be able to determine which investigations, if any, are relevant.
79% of asymptomatic adults between 50 and 65 have radiological abnormalities of the spine which do not warrant any intervention. (3) For this reason, there is no indication for any imaging or work-up in the first 6 weeks for a patient presenting with low back pain without worrisome features (Table 1). (4)
It is indicated to image the patient starting with an X-ray in cases of trauma, worsening neurologic deficit, or when an infection or a malignancy is suspected. (3) Further imaging such as a computed tomography (CT) or a magnetic resonance imaging (MRI) may be the next step if an X-ray does not allow a diagnosis or if a pathology involving the spinal canal is suspected.
If an evident fracture is identified, expert consultation is warranted to rule out instability and the need for surgery. If a CT or MRI reveal an infection, neural compression, malignancy or infection, urgent expert consultation is necessary.
The role of laboratory tests in lower back pain is to identify infectious and malignant causes. An elevated c-reactive protein (CRP), white blood cell count (WBC), and erythrocyte sedimentation rate (ESR) and the presence of fever are suggestive of an infective etiology. (5) In cases where a multiple myeloma is suspected, the best initial test is a serum protein electrophoresis. (6)
Beyond the initial approach
Managing Lower back pain
In 75% to 90% of patients, acute lower back pain improves within a month. (7) Initial management of the patient suffering from lower back pain without worrisome features includes three key spheres of intervention: reassuring and educating the patient, pharmacological interventions, and physical interventions.
It is important to explain to the patient with simple lower back pain that the condition is likely to improve by itself and to reassure them of the benign and widespread nature of the condition. Immobilization should be discouraged, and the patient should be recommended to stay active and limit time off from work in order to reduce long-term disability and accelerate recovery. (8)
Non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen seem to offer a mild effect in short-term pain reduction and disability. (9) (10) Muscle relaxants and narcotics offer no benefit in short-term pain relief compared to NSAIDS and acetaminophen, and multiple studies have raised concerns with regards to their side effects and risks. (11)
Physical treatment modalities proven to improve lower back pain and increase function include physical therapy, spinal manipulation by trained specialists (12), and active mobilization exercises such as tai chi, yoga or any other prescribed exercises. All these methods are safe and effective, but spinal manipulation appears to offer a larger benefit than mobilization in regards to pain reduction and functional improvement in chronic lower back pain patients. (13) Application of cold or warm compress to the painful region is safe and may result in a mild improvement in symptoms. There is insufficient evidence to favor the use of one over the other. (14) Acupuncture for non-specific lower-back pain remains unproven. (15) In summary, physical treatment modalities should be used as often as possible as they are safe, cost efficient, and associated with high patient satisfaction and symptom improvement. (16)
Conclusion
A recent systematic review estimated the global point prevalence of activity-limiting low back pain lasting for more than one day was 12% and the one-month prevalence was 23%. (17) This common condition accounts for many primary-care consultations and is self-limited in most cases. Due to the high number of asymptomatic individuals with radiological anomalies, imaging is reserved for cases of trauma or when malignancy, infection, or neural compromise are suspected. Treatment of lower back pain focuses on alleviating the acute symptoms and preventing chronicity by educating the patient, favoring physical treatments, and providing symptom management with NSAIDS and/or acetaminophen while limiting the use of narcotics or muscle relaxants.
References
- Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med [Internet]. 2002 Oct 1 [cited 2021 Mar 9];137(7):586–97. Available from: https://pubmed-ncbi-nlm-nih-gov.proxy3.library.mcgill.ca/12353946/
- Sun JC, Xu T, Chen KF, Qian W, Liu K, Shi JG, et al. Assessment of cauda equina syndrome progression pattern to improve diagnosis. Spine (Phila Pa 1976) [Internet]. 2014 Apr 1 [cited 2021 Mar 9];39(7):596–602. Available from: https://pubmed-ncbi-nlm-nih-gov.proxy3.library.mcgill.ca/24150427/
- Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic Resonance Imaging of the Lumbar Spine in People without Back Pain. N Engl J Med [Internet]. 1994 Jul 14 [cited 2020 Dec 12];331(2):69–73. Available from: https://pubmed.ncbi.nlm.nih.gov/8208267/
- Chou R. Diagnostic Imaging for Low Back Pain: Advice for High-Value Health Care From the American College of Physicians. Ann Intern Med [Internet]. 2011 Feb 1 [cited 2020 Dec 12];154(3):181. Available from: http://annals.org/article.aspx?doi=10.7326/0003-4819-154-3-201102010-00008
- Nasser MJ. How to approach the problem of low back pain: an overview. J Family Community Med [Internet]. 2005 Jan [cited 2020 Dec 12];12(1):3–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23012066
- Tripathy S. The role of serum protein electrophoresis in the detection of multiple myeloma: An experience of a corporate hospital. J Clin Diagnostic Res [Internet]. 2012 Nov 15 [cited 2020 Dec 12];6(9):1458–61. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3527769/
- Atlas SJ, Deyo RA. Evaluating and managing acute low back pain in the primary care setting. J Gen Intern Med [Internet]. 2001 Feb [cited 2020 Dec 12];16(2):120–31. Available from: /pmc/articles/PMC1495170/?report=abstract
- Koes BW, Van Tulder MW, Thomas S. Diagnosis and treatment of low back pain [Internet]. Vol. 332, British Medical Journal. BMJ Publishing Group; 2006 [cited 2020 Dec 12]. p. 1430–4. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1479671/
- van der Gaag WH, Roelofs PDDM, Enthoven WTM, van Tulder MW, Koes BW. Non-steroidal anti-inflammatory drugs for acute low back pain [Internet]. Vol. 2020, Cochrane Database of Systematic Reviews. John Wiley and Sons Ltd; 2020 [cited 2020 Dec 12]. Available from: https://pubmed.ncbi.nlm.nih.gov/32297973/
- Research SB-A for HCP and, Public undefined, 1994 undefined. Acute low back problems in adults. Clinical practice guideline No 14. ci.nii.ac.jp [Internet]. [cited 2020 Dec 12]; Available from: https://ci.nii.ac.jp/naid/10018101252/
- van Tulder MW, Touray T, Furlan AD, Solway S, Bouter LM. Muscle relaxants for non-specific low-back pain. Cochrane Database Syst Rev [Internet]. 2003 Apr 22 [cited 2020 Dec 12];2017(3). Available from: http://doi.wiley.com/10.1002/14651858.CD004252
- Shekelle PG, Adams AH, Chassin MR, Hurwitz EL, Brook RH. Spinal manipulation for low-back pain [Internet]. Vol. 117, Annals of Internal Medicine. American College of Physicians; 1992 [cited 2020 Dec 12]. p. 590–8. Available from: https://pubmed.ncbi.nlm.nih.gov/1388006/
- Coulter ID, Crawford C, Hurwitz EL, Vernon H, Khorsan R, Suttorp Booth M, et al. Manipulation and mobilization for treating chronic low back pain: a systematic review and meta-analysis [Internet]. Vol. 18, Spine Journal. Elsevier Inc.; 2018 [cited 2020 Dec 12]. p. 866–79. Available from: https://pubmed.ncbi.nlm.nih.gov/29371112/
- Garra G, Singer AJ, Leno R, Taira BR, Gupta N, Mathaikutty B, et al. Heat or cold packs for neck and back strain: A randomized controlled trial of efficacy. Acad Emerg Med [Internet]. 2010 [cited 2020 Dec 12];17(5):484–9. Available from: https://pubmed.ncbi.nlm.nih.gov/20536800/
- Van Tulder MW, Gherkin DC, Berman B, Lao L, Koes BW. The effectiveness of acupuncture in the management of acute and chronic low back pain: A systematic review within the framework of the cochrane collaboration back review group [Internet]. Vol. 24, Spine. Spine (Phila Pa 1976); 1999 [cited 2020 Dec 12]. p. 1113–23. Available from: https://pubmed.ncbi.nlm.nih.gov/10361661/
- Carey TS, Garrett J, Jackman A, McLaughlin C, Fryer J, Smucker DR. The Outcomes and Costs of Care for Acute Low Back Pain among Patients Seen by Primary Care Practitioners, Chiropractors, and Orthopedic Surgeons. N Engl J Med [Internet]. 1995 Oct 5 [cited 2020 Dec 12];333(14):913–7. Available from: https://pubmed.ncbi.nlm.nih.gov/7666878/
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain [Internet]. Vol. 64, Arthritis and Rheumatism. Arthritis Rheum; 2012 [cited 2021 Mar 9]. p. 2028–37. Available from: https://pubmed-ncbi-nlm-nih-gov.proxy3.library.mcgill.ca/22231424/

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.