Approach to
Delirium
Alfiya Mukharyamova1
Published online: October 13, 2021
1McGill University
Corresponding Author: Alfiya Mukharyamova, email alfiya.mukharyamova@mail.mcgill.ca
DOI: 10.26443/mjm.v20i2.813
Abstract
Delirium is a common and serious geriatric syndrome with core features of acute onset and inattention. This syndrome is often underdiagnosed and is associated with many adverse outcomes, such as prolonged hospitalization, institutionalization, functional impairment and death. This review summarizes an approach to the recognition, work-up, management and prevention of delirium.
Tags: Delirium
Question
An 82-year-old woman is admitted with a hip fracture. Past medical history is remarkable for hypertension, for which she takes amlodipine and perindopril, and occasional constipation. She lives at home with her partner and is independent for all her activities of daily living. Her intraoperative course is unremarkable, but on postoperative day 2 she develops agitation and confusion. Her vital signs are notable for a blood pressure of 160/100 mmHg and tachycardia of 105 bpm, the other findings in a limited physical exam are normal. Her complete blood count, serum electrolytes and urinalysis are normal this morning.
Which intervention is considered first-line in this situation?
- Physical restraints
- Haloperidol
- Quetiapine
- Analgesics
- Diazepam
Answer
D. The initial management for delirium involves addressing the underlying condition and utilizing non-pharmacologic interventions. In this case, once life-threatening conditions are ruled out, uncontrolled pain likely precipitated the patient’s delirium (1). However, caution needs to be taken when using analgesics in older adults; scheduled adjuvant treatments should be used to minimize the use of opioids (2). The use of physical restraints should be limited as this is associated with an increased risk of injury (3). Antipsychotic medications such as haloperidol and quetiapine should only be considered if distressing symptoms or dangerous behaviour is present and if non-pharmacologic measures have failed (2,4). Benzodiazepines such as diazepam have consistently been associated with poorer outcomes in older adults and, in general, should only be used in cases of alcohol withdrawal or if the patient has a history of neuroleptic malignant syndrome and therefore cannot take antipsychotics (2).
Initial approach
Recognition of delirium
Delirium was often described using a diverse range of terms such as “acute confusional state”, “toxic metabolic encephalopathy” and “acute brain syndrome” (5). Over time, the definition has evolved to describe an acute and fluctuating syndrome of reduced awareness and inability to sustain attention, usually occurring in the setting of a medical condition (6). Though delirium typically develops over a short period of time, it can persist for weeks or even months, and it is “not better accounted for by a pre-existing, established, or evolving dementia” (7).
Risk factors for developing delirium include advanced age, regular administration of more than 5 medications, presence of cognitive or sensory impairments and presence of multiple co-morbidities (1).
Delirium is a clinical diagnosis and multiple scales have been developed to aid clinicians in recognizing this syndrome. A commonly used validated scale is the Confusion Assessment Method (CAM), which has a sensitivity of 94-100\% and a specificity of 90-95\% (8). The diagnosis of delirium by CAM requires the presence of acute onset with fluctuating course and inattention, and either disorganized thinking or an altered level of consciousness (Table 1). Inattention is commonly assessed using various bedside tests. Examples of such tests include: the digit span test—patients are asked to recall the sequence of numbers; reciting the months of the year and days of the week backward; and serial sevens—counting down from one hundred in sevens (9). Although these tests are helpful in diagnosing delirium, a positive response to the following: "Did the patient have difficulty focusing attention, for example, being easily distractible or having difficulty keeping track of what was being said?" is sufficient to diagnose delirium with the CAM model.
| Table 1: The Confusion Assessment Method (CAM) | Feature | Assessment |
| 1. Acute onset and fluctuating course | Usually obtained from a family member or nurse and shown by positive responses to the following questions: "Is there evidence of an acute change in mental status from the patient's baseline?" and "Did the abnormal behavior fluctuate during the day, that is, tend to come and go, or increase and decrease in severity?" |
| 2. Inattention | Shown by a positive response to the following: "Did the patient have difficulty focusing attention, for example, being easily distractible or having difficulty keeping track of what was being said?" |
| 3. Disorganized thinking | Shown by a positive response to the following: "Was the patient's thinking disorganized or incoherent, such as rambling or irrelevant conversation, unclear or illogical flow of ideas, or unpredictable switching from subject to subject?" |
| 4. Altered level of consciousness | This feature is shown by any answer other than "alert" to the following question: Overall, how would you rate this patient's level of consciousness? (alert [normal], vigilant [hyperalert], lethargic [drowsy, easily aroused], stupor [difficult to arouse], or coma [unarousable]) |
Delirium is often missed in a busy hospital setting, particularly if the patient is only seen briefly and happens to be in a lucid interval. Additionally, delirium can present with either hyperactive features such as restlessness, agitation, and hypervigilance; or hypoactive features such as lethargy and sedation (6). The fact that hypoactive delirium is more common that hyperactive delirium creates additional diagnostic challenges (10). Rates of unrecognized delirium, defined as delirium diagnosed by an expert assessor after the diagnosis was not made by the patient’s treating physicians and nurses, are around 60\% (11). Hence, clinicians and trainees should remain vigilant when the patient is described as “confused” or “not themselves” and gather collateral information from other healthcare professionals and family members. Delirium superimposed on dementia (DSD) poses another diagnostic challenge, since clinical phenotypes of some dementias show overlap with delirium. More research is needed to develop better tools for diagnosis of DSD (12).
Identifying the cause
Once delirium has been recognized, clinicians should aim to identify and treat the underlying etiology. The majority of recommendations for the evaluation and treatment of delirium are based on clinical observations and expert opinion since there are currently no laboratory or radiological studies available to confirm its presence and resolution (1).
There are various mnemonics and system-based approaches to help clinicians identify the precipitant of delirium. One commonly used mnemonic, DELIRIUM, is outlined in Table 2 (2). This mnemonic includes the following causes of delirium to consider: drugs; electrolyte and endocrine disturbances; lack of drugs, i.e. discontinuation of drugs; infections; reduced sensory input; intracranial disorders; urinary and fecal disorders; and myocardial and pulmonary disorders as causes of delirium to consider. Given a wide differential diagnosis and frequent “atypical” presentations of diseases in older adults, a clinician must develop a systematic approach to any patient experiencing delirium, as briefly summarized below.
| Table 2: Common Causes of Delirium | Category | Examples to consider | |
| D - drugs | Newly initiated drugs, changed doses, interactions, including over the counter drugs | ||
| E - electrolyte and endocrine disturbances | Common imbalances include dehydration, sodium and calcium imbalance, and thyroid issues | ||
| L - lack of drugs | Recently discontinued medications and substances that can cause withdrawal symptoms or increased pain levels | ||
| I - infections | Urinary tract, respiratory tract, soft tissue, and device infections | ||
| R - reduced sensory input | Lack of hearing and vision aid | ||
| I - intracranial disorders | Strokes, bleeds, masses | ||
| U - urinary and fecal disorders | Urinary retention and constipation | ||
| M - Myocardial and pulmonary disorders | Myocardial infarcts, arrhythmias, hypoxia, hypercapnia | ||
History
Clinicians should inquire as to: when the mental status changes first began; how they change throughout the day; and whether they are associated with other physical signs and symptoms, for example, tachypnea. A thorough review of medications, over the counter drugs, and other substances is required as well (2). Consideration should also be given to recently discontinued medications and substances that may cause withdrawal, such as alcohol or benzodiazepines.
Physical Exam
Physical exam should include measurement of vital signs, hydration status, skin condition, and should evaluate for potential infectious foci. An examination of the cardiovascular, respiratory and abdominal systems should be performed. If possible, a neurological exam should be performed to evaluate for new focal findings (2).
Laboratory tests
Targeted testing based upon history and physical exam is appropriate in most cases, as desire for diagnostic completeness can increase costs, subject patients to unnecessary investigations and potentially delay the diagnosis or more obvious disorders (13). However, a thorough review of all differential diagnoses should be performed, particularly to rule out life-threatening causes such as hypoglycemia and medication toxicities in a timely manner. Routine laboratory tests include a complete blood count, measurement of serum electrolytes, venous blood gas, liver-function tests, and urinalysis and urine culture (2). Chest radiograph, electrocardiogram, and troponins are also often helpful (2). Additional tests that may be required include screening for toxicology and specific drugs (e.g. digoxin, lithium); blood cultures; and more extensive imaging, for example, computed tomography of the head (2). Lumbar puncture and electroencephalography are rarely helpful unless there is a high clinical suspicion of meningitis or seizure activity, respectively (2).
Management and prevention
Management of delirium is a complex process that often requires interdisciplinary teams (2). Although the focus is on addressing the underlying cause such as a urinary tract infection or contribution from a medication, the prevention of complications and maintenance of patient comfort and safety are as important. Strategies to minimize complications include monitoring urine output and bowel movements, avoiding physical restraints, ensuring adequate dietary intake, and appropriate mobilization (2).
Non-pharmacologic interventions remain the cornerstone of delirium management, as most studies do not show benefit of antipsychotic medications on decreasing the duration and severity of delirium, and multiple studies demonstrate harm with the use of such medications (14). Some of the non pharmacological interventions include: correction of hearing and vision deficits; appropriate mobilization; improvement of sleep-wake cycles with exposure to daylight during the day and minimization of noise and disruptions during the nighttime; orientation activities; and avoidance of abrupt changes in patient’s environment, for example, frequent room changes (15). Early efforts to restore function should include involvement of physical and occupational therapy specialists to optimize activities of daily living (2).
Family education can also be beneficial both to the patient and to the caregiver. For example, family education allows caregivers to recognize subtle changes in cognition, which can be helpful in the diagnosis of delirium. Close knowledge regarding the patient’s needs, routines, and manifestations of discomfort can also be utilized to provide earlier detection and treatment. Furthermore, family can often help with non-pharmacological management, such as re-orienting the patient using familiar objects (15).
With increased awareness of how prevalent delirium is within the hospital settings, many interventions have been developed in attempts to prevent delirium. One of the most widely disseminated interventional programs is the Hospital Elder Life Program (HELP) (16). HELP uses trained volunteers to provide patients with individually assigned interventions such as (re-)orientation, cognitive activation, mobilization, meal companionship, and hydration. This program has been shown to significantly reduce the rates of delirium and prevent loss of functioning in hospitalized older adults (16,17).
Beyond Initial Approach
Pharmacologic therapies may sometimes be required for distressing sensory disturbances or behaviours that can pose danger to the patient or others (2). Low dose, short term therapy with haloperidol or an atypical antipsychotic (e.g. risperidone) can be considered, though the use of antipsychotics for management of delirium is considered an off-label indication in Canada (18). These drugs are contra-indicated in patients with Parkinson disease, Lewy body dementia, and history of neuroleptic malignant syndrome. Such agents can significantly worsen parkinsonism and cognitive impairment and significantly increase the risk of mortality (19).
Benzodiazepines are considered second-line agents and should only be used in cases of alcohol withdrawal or if the patient has a history of neuroleptic malignant syndrome and therefore should not take antipsychotics (2). Large studies have consistently showed poor outcomes associated with benzodiazepine use in older adults (20).
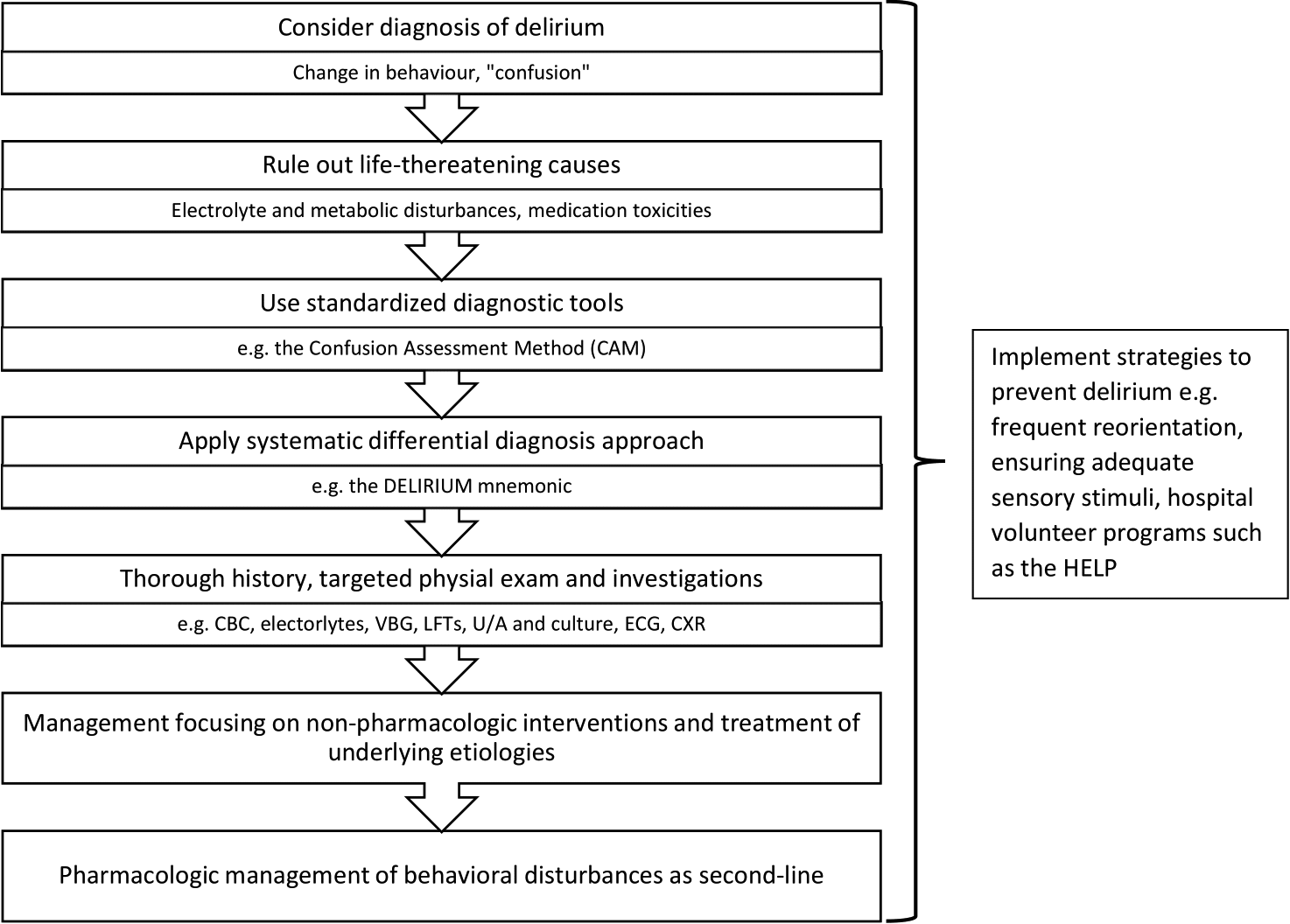
CBC - complete blood count, VBG – venous blood gas, LFTS - liver function tests, U/A - urinalysis, ECG - electrocardiogram, CXR – chest X-ray, HELP - Hospital Elder Life Program
References
- Setters B, Solberg LM. Delirium. Prim Care. 2017 Sep;44(3):541–59.
- Marcantonio ER. Delirium in Hospitalized Older Adults. New England Journal of Medicine. 2017 Oct 12;377(15):1456–66.
- American Geriatrics Society Expert Panel on Postoperative Delirium in Older Adults. American Geriatrics Society abstracted clinical practice guideline for postoperative delirium in older adults. J Am Geriatr Soc. 2015 Jan;63(1):142–50.
- Canadian Geriatrics Society list of 5 things physicians and patients should question in geriatrics [Internet]. Choosing Wisely Canada. [cited 2020 Nov 22]. Available from: https://choosingwiselycanada.org/geriatrics/
- Morandi A, Pandharipande P, Trabucchi M, Rozzini R, Mistraletti G, Trompeo AC, et al. Understanding international differences in terminology for delirium and other types of acute brain dysfunction in critically ill patients. Intensive Care Med. 2008 Oct;34(10):1907–15.
- Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009 Apr;5(4):210–20.
- The DSM-5 criteria, level of arousal and delirium diagnosis: inclusiveness is safer. BMC Med [Internet]. 2014 Sep 25 [cited 2020 Nov 22];12. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4177077/
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990 Dec 15;113(12):941–8.
- Tieges Z, Brown LJE, MacLullich AMJ. Objective assessment of attention in delirium: a narrative review. Int J Geriatr Psychiatry. 2014 Dec;29(12):1185–97.
- Inouye SK, Westendorp RGJ, Saczynski JS. Delirium in elderly people. Lancet. 2014 Mar 8;383(9920):911–22.
- Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in Older Persons: Advances in Diagnosis and Treatment. JAMA. 2017 26;318(12):1161–74.
- Morandi A, Davis D, Bellelli G, Arora RC, Caplan GA, Kamholz B, et al. The Diagnosis of Delirium Superimposed on Dementia: An Emerging Challenge. J Am Med Dir Assoc. 2017;18(1):12–8.
- Diagnosis of delirium and confusional states - UpToDate [Internet]. [cited 2020 Nov 22]. Available from: https://www.uptodate.com/contents/diagnosis-of-delirium-and-confusional-states?search=delirium&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- Inouye SK, Marcantonio ER, Metzger ED. Doing Damage in Delirium: The Hazards of Antipsychotic Treatment in Elderly Persons. Lancet Psychiatry. 2014 Sep 1;1(4):312–5.
- Boland JW, Link to external site this link will open in a new window, Lawlor PG, Bush SH, Link to external site this link will open in a new window. Delirium: non-pharmacological and pharmacological management. BMJ Supportive & Palliative Care. 2019 Dec;9(4):482–4.
- Inouye SK, Bogardus ST, Charpentier PA, Leo-Summers L, Acampora D, Holford TR, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999 Mar 4;340(9):669–76.
- Hshieh TT, Yang T, Gartaganis SL, Yue J, Inouye SK. Hospital Elder Life Program: Systematic Review and Meta-analysis of Effectiveness. Am J Geriatr Psychiatry. 2018 Oct;26(10):1015–33.
- Rios S, Perlman CM, Costa A, Heckman G, Hirdes JP, Mitchell L. Antipsychotics and dementia in Canada: a retrospective cross-sectional study of four health sectors. BMC Geriatr [Internet]. 2017 Oct 23 [cited 2020 Nov 22];17. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5651600/
- McKeith IG, Perry RH, Fairbairn AF, Jabeen S, Perry EK. Operational criteria for senile dementia of Lewy body type (SDLT). Psychol Med. 1992 Nov;22(4):911–22.
- Bush SH, Lawlor PG. Delirium. CMAJ. 2015 Feb 3;187(2):129–129.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.