Approach to
Pneumonia in Immunocompetent Patients
Spandana Veeravalli1, Safiya Soullane1
Published online: 25 June 2021
1Faculty of Medicine, McGill University, Montreal, QC, Canada
Corresponding Author: Spandana Veeravalli, email spandana.veeravalli@mail.mcgill.ca
DOI: 10.26443/mjm.v20i2.511
Abstract
Pneumonia is a leading cause of morbidity. Pneumonia is defined as a lung inflammation of infectious etiology. It can be subcategorized into Community Acquired Pneumonia, Hospital Acquired Pneumonia and Ventilator Acquired Pneumonia. Validated scores including the CRB-65, CURB-65 and PSI can guide decision-making between inpatient and outpatient management of pneumonia. While mild presentations can be managed through empiric treatment alone, more acute cases require identification of the infectious agent, initiation of empiric therapy, and subsequent de-escalation of treatment to the identified pathogen. This article aims to provide a framework for junior trainees to diagnose and manage pneumonia.
Tags: Geriatrics, Fall, Elderly
Question
A 66-year-old male presents to the emergency room with a history of non-productive cough for the past five days. The patient also reports subjective fever for the past five days, and shortness of breath for the past three days. He explains that initially his symptoms were mild and tolerable but have gotten progressively worse since yesterday, prompting him to seek medical attention today. He has known hypertension, for which he takes ramipril. His past medical history is otherwise unremarkable, and he has no recent travel history.
On examination, he is alert and oriented, slightly tachycardic (108 bpm), tachypneic (29 breaths/min), with an O2 saturation of 93% and a slightly elevated blood pressure (129 mmHg / 88 mmHg). He appears fatigued. Auscultation reveals wheezing. Oral temperature is 38.4°C. His chest radiograph shows evidence of a diffuse pulmonary infiltrate.
Assuming the most likely diagnosis, what would you do next?
- Admit him to the hospital and treat with levofloxacin
- Obtain sputum gram stain and culture
- Treat out-patient with azithromycin
- Treat out-patient with gentamicin
- Treat out-patient with levofloxacin
Answer
C. The patient’s symptoms are consistent with community acquired pneumonia (CAP), with the pulmonary infiltrates on chest x-ray further increasing the likelihood of this diagnosis. The patient’s CRB-65 score is 1. Given that the point was attributed due to the age criterion, he does not need a hospital admission. For outpatient care of community acquired pneumonia, empiric treatment is often sufficient. Azithromycin is a good broad-spectrum antibiotic that will cover common CAP pathogens such as Streptococcus pneumoniae. Gentamicin only covers gram-negative bacteria and is therefore inadequate for CAP treatment. Fluoroquinolones such as levofloxacin are not recommended as first-line therapy for out-patient treatment of community acquired pneumonia. (1)
This article aims to provide an initial approach to pneumonia for junior trainees. The data presented follows guidelines from Quebec (Canada) and may not be applicable to other settings.
Initial Approach
Pneumonia is defined as a lung inflammation caused by an infection of bacterial, viral or fungal etiology. (1) Host immunity, pathogen virulence and inoculum size interplay to modulate the risk of pneumonia. Routes of infection include micro-aspiration, macro-aspiration and hematogenous spread. (2) The most common symptoms are cough, sputum production, dyspnea, pleuritic chest pain, and deterioration in overall health. Common physical examination findings include tachypnea, tachycardia, fever, low oxygen saturation, dullness on percussion, diminished breath sounds, rales and/or rhonchi. (3)
Diagnosis
The most commonly ordered test when investigating pneumonia is the chest radiograph (posteroanterior and lateral views). (4) Radiographic findings suggestive of pneumonia include lobar consolidates, pulmonary infiltrates, and/or cavitations. (4) The presence of cavitations indicates tissue necrosis and the development of lung abscesses. In cases of upper lobe cavitations, clinicians must be cautious to rule out Mycobacterium tuberculosis. (5)
While chest radiograph (CXR) is the standard imaging test, it has some limitations including poor image quality. (6) Other diagnostic modalities include chest computerized tomography (CT) and lung ultrasound. (6) Although CT scan is more precise and may identify pneumonias that are not detected on CXR, it is associated with increased costs and exposure to radiation. (6) Lung ultrasound may be useful for bedridden and unstable patients for whom it may be difficult to obtain a CXR. (7)
Sputum cultures are warranted for all hospitalized patients with severe illness. (8) However, they have been shown to be effective in identifying the infectious etiology only about half of the time. (8) Rapid molecular tests such as PCR and LAMP have been shown to be promising techniques that would improve testing turnaround time and sensitivity. (8) Yet, some issues still remain in terms of the diagnostic capacity of these tests, and cost effectiveness studies are needed before they are put to use more widely. (8)
Classification
Pneumonia can be subcategorized into three different diagnoses based on the context of acquisition: Community Acquired Pneumonia (CAP), Hospital Acquired Pneumonia (HAP), and Ventilator Acquired Pneumonia (VAP). (9) CAP is defined as the development of pneumonia symptoms outside of a hospital setting, or within the first 48 hours of hospitalization. If symptoms occur past the first 48 hours of hospitalization, the appropriate diagnosis is HAP. The third diagnosis, VAP, is defined by symptom development occurring 48 hours after intubation. (9)
Community Acquired Pneumonia
CAP is a leading cause of hospitalization and morbidity. (1, 3) The most commonly isolated agent is Streptococcus pneumoniae. Other pathogens include influenza A virus, Mycoplasma pneumoniae and Chlamydophila pneumoniae. (3) While respiratory viruses, typical bacteria and atypical bacteria are the most common identified etiologies, the pathogen is unidentifiable in up to 60% of CAP cases. (10) Suspicion of a causative agent should be based on the region, season, and patient risk factors. (11)
While the choice between inpatient and outpatient care is usually made by using clinical judgment, validated scores can help support this decision. (3, 12) Previous research reports that the CRB-65, CURB-65 and PSI scores are comparable in predicting mortality, (12) although some data suggests PSI has a stronger predictive power for 30-day mortality. (4) The CRB-65 does not require invasive testing and is simpler to apply. (4) The CURB-65 may be favorable if bloodwork is being ordered, and/or is easily accessible. (4, 11) Evidence suggests that PSI is more accurate for low-risk patients, although it requires more intricate testing including arterial blood gas. (11, 12) All things considered, the use of CRB-65 is favorable in primary care settings. (3, 4) Patients needing hospital admission can further be triaged between a general ward and an ICU admission, according to the criteria listed in IDSA/ATS guidelines. (1) See Table 1 for complementary information.
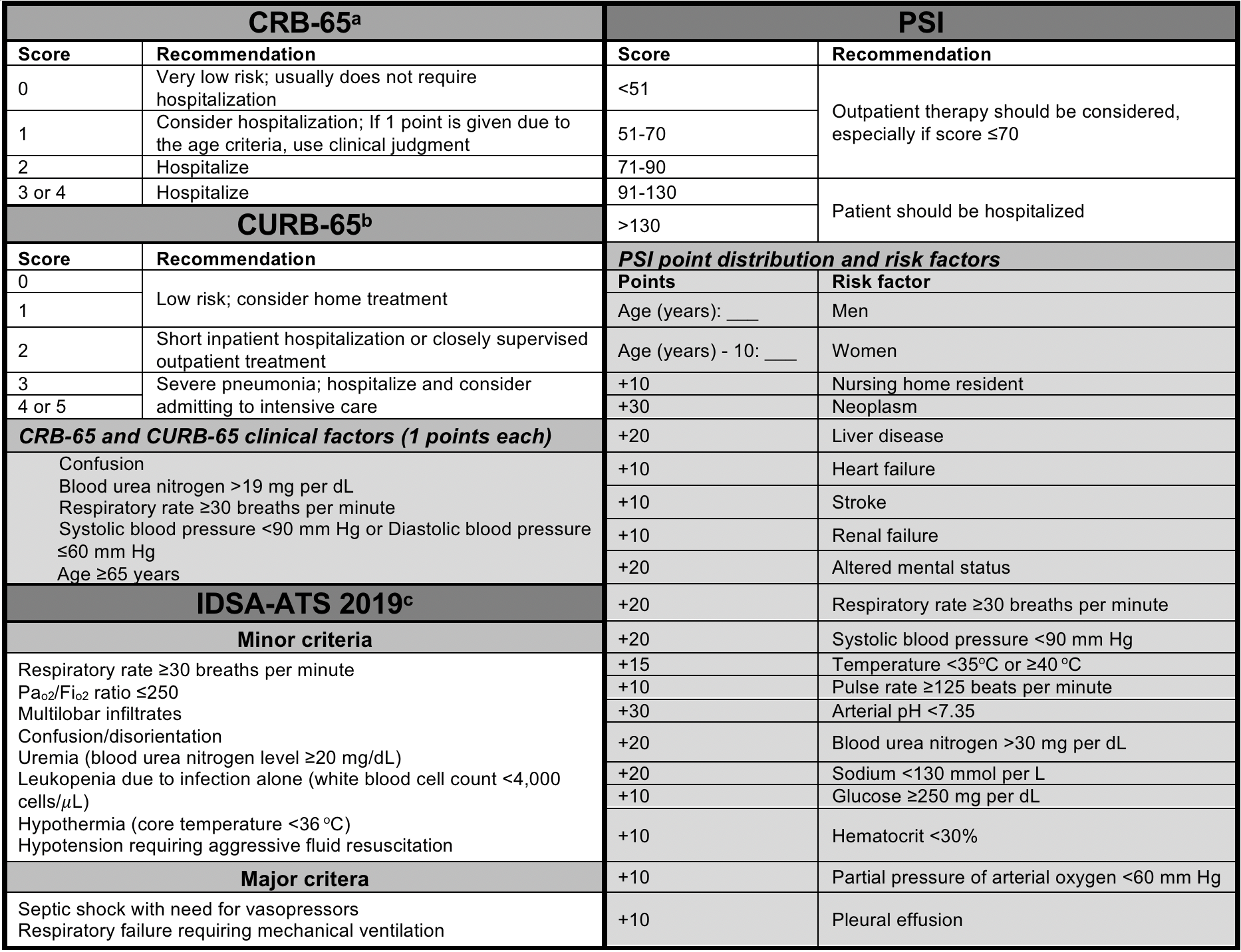
aCRB-65 - Confusion, Respiratory rate, Blood pressure, 65 years of age and older.
bCURB-65 - Confusion, Urea nitrogen, Respiratory rate, Blood pressure, 65 years of age and older.
cIDSA-ATS 2019 guidelines - Patients should be considered for ICU admission if they satisfy either =1 major criteria, or =3 minor criteria.
Adapted from:
Institut national d’excellence en santé et en services sociaux. Pneumonie acquise en communauté chez l’adulte [Internet]. 2017. Available from: https://www.inesss.qc.ca/fileadmin/doc/CDM/UsageOptimal/Guides-serieI/INESSS_Annexes_Rapport_GUO_PAC.pdf.
Watkins RR, Lemonovich TL. Diagnosis and Management of Community-Acquired Pneumonia in Adults. AFP. 2011; 83(11):1299–306.
Guidelines for Treatment
Once diagnosis and choice of hospital admission have been made, treatment may be initiated. Examples of first-line therapy for outpatient care include select macrolides, tetracyclines and ß-lactams. If no improvement is observed after 72 hours of therapy, respiratory fluoroquinolones are suggested as second-line options. (3) Since certain conditions can increase the risk of severe illness, antibiotic choice also depends on the presence of patient risk factors (Table 2).
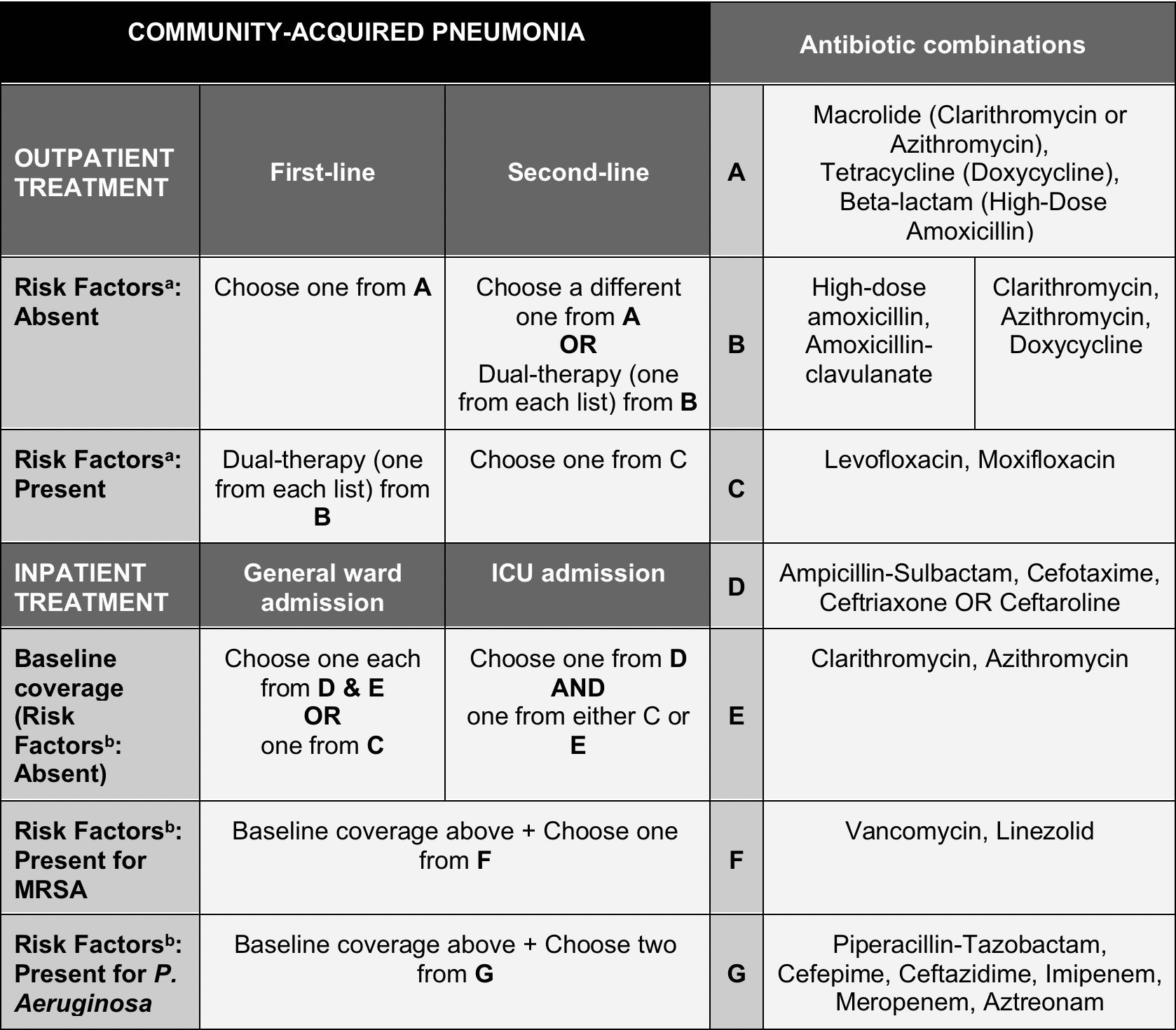
aOutpatient: Risk factors to consider include smoking; antibiotic use in the past 90 days; chronic heart, lung, kidney, or liver disease; diabetes mellitus; alcohol dependence; immunosuppression.
bInpatient: Specific risk factors for MRSA or P. Aeruginosa include: Previous infection with the pathogen, recent hospitalization, recent use of parenteral antibiotics, site-specific risk factors for either pathogen.
Adapted from:
Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019; 200(7):e45–67.
For inpatient treatment, the recommended approach is based on the severity of the disease, with patients admitted to the ICU and those with risk factors receiving more intensive treatment with multiple drugs. (1, 4) It is recommended to order a sputum gram stain and culture, if possible, prior to initiating empiric therapy for CAP patients with severe presentations. (1)
Further information on treatment choice, as well as the complete list of patient risk factors, is compiled in Table 2. See Figure 1 for management flow chart.
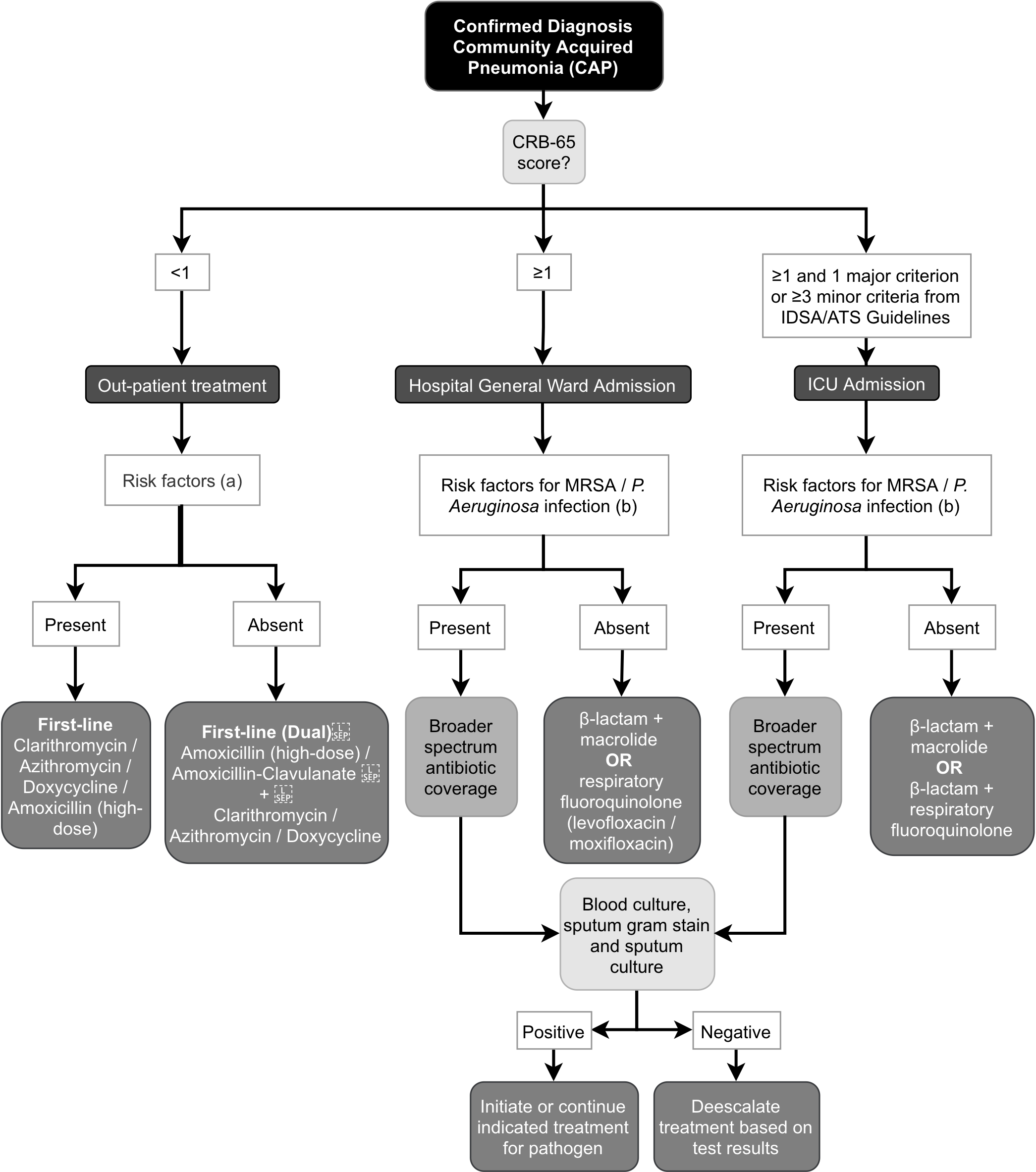
aOutpatient: Risk factors to consider include smoking; antibiotic use in the past 90 days; chronic heart, lung, kidney, or liver disease; diabetes mellitus; alcohol dependence; immunosuppression.
bInpatient: Specific risk factors for MRSA or P. aeruginosa include (10):
- Previous infection with the pathogen
- Recent hospitalization
- Recent use of parenteral antibiotics
- Site-specific risk factors for either pathogen
Adapted from:
Institut national d’excellence en santé et en services sociaux. Pneumonie acquise en communauté chez l’adulte [Internet]. 2017. Available from: https://www.inesss.qc.ca/fileadmin/doc/CDM/UsageOptimal/Guides-serieI/INESSS_Annexes_Rapport_GUO_PAC.pdf.
Kumar ST, Yassin A, Bhowmick T, Dixit D. Recommendations From the 2016 Guidelines for the Management of Adults With Hospital-Acquired or Ventilator-Associated Pneumonia. P T. 2017; 42(12):767–72.
Hospital Acquired Pneumonia
Admitted patients have an increased exposure to pathogens of the hospital environment. Direct contact with care providers, as well as intubation, tracheostomy, and other respiratory interventions can facilitate the spread of pathogens and increase risks of HAP. The most commonly isolated pathogens include gram-negative bacilli and Staphylococcus aureus, and clinicians should maintain a high suspicion for drug-resistant organisms. (13)
Guidelines for Treatment
The main risk factor for a drug-resistant pathogen infection in HAP patients is antibiotic use in the past 90 days. (14) Clinicians must be cautious of the development of septic shock and need for ventilatory support secondary to pneumonia, as they have been associated with mortality. (13, 14)
In stable patients with HAP, physicians usually opt to order a sputum culture prior to initiating empiric therapy. (14) It is recommended that empiric treatment regimens be based on local or site-specific data regarding HAP-associated pathogens and corresponding antibiograms. All empiric treatment regimens for HAP should ideally cover pathogens such as S. aureus, and P. aeruginosa or other gram-negative bacilli. Aminoglycoside monotherapy should be avoided due to toxicity and poor lung penetration. (14)
Ventilator Acquired Pneumonia
For VAP, important routes of infection include microaspiration and tracheal tube contamination. Bacteria form biofilms inside the tracheal tube and contaminate oropharyngeal secretions. As the tube is introduced into the airways, pathogens reach the lung parenchyma and replicate. (15) While the main causative agent is Pseudomonas aeruginosa, other common pathogens include Escherichia coli, Klebsiella pneumoniae, and Acinetobacter, as well as gram-positive cocci such as S. aureus. (13)
Guidelines for Treatment
Risk factors for a multidrug-resistant pathogen infections in VAP patients include: intravenous antibiotic use in the past 90 days, septic shock at the time of pneumonia onset, acute respiratory distress syndrome, =5 days of hospitalization, and acute renal replacement therapy prior to pneumonia onset. (14)
Similar to HAP, stable VAP patients should have bacterial cultures ordered prior to initiation of empiric treatment. The recommended lab investigation, in this case, is a semiquantitative culture of an endotracheal aspirate (ETA). This test was found to be the most sensitive when compared to other testing options for intubated patients (e.g. quantitative ETA, quantitative bronchoalveolar lavage, etc.). (14)
Empiric treatment regimens should be chosen according to local or site-specific data on VAP-associated pathogens and corresponding antibiograms. Empiric treatment regimens for VAP should cover pathogens such as S. aureus, and P. aeruginosa or other gram-negative bacilli. It is also recommended that the use of aminoglycosides and colistin be avoided. (14)
Beyond the Initial Approach
Considerations for Management
Whenever bacterial cultures are ordered prior to initiation of empiric therapy, treatment should be de-escalated to target the isolated pathogen. (1, 14) Since pneumonia is a presentation that can frequently lead to sepsis, blood cultures should be ordered to investigate bacteremia in severe presentations. (16)
Due to the association of pneumonia and pleural disease, clinicians must also be cautious of the development of effusion and empyema in patients not improving despite treatment. In these conditions, the patient may require invasive interventions including tube thoracostomy. (17)
For CAP, the course of antibiotics should last >5 days as a general rule. (1) For HAP and VAP, the recommended treatment duration is 7 days. (14) In all cases, treatment should only be discontinued once the patient reaches clinical stability. (1, 14)
The following evidence-based measures may be used to evaluate the patient’s clinical stability: ability to eat, normal mentation, and vital signs including heart rate, respiratory rate, blood pressure, oxygen saturation, and temperature. (1) Procalcitonin levels may also be useful to determine if antibiotics should be discontinued, especially in patients with HAP or VAP. (14)
Epidemic Pathogens
Additional tests may be recommended if the patient is suspected to have been exposed to epidemic pathogens. To identify influenza, a molecular assay test is recommended. In influenza positive patients, it is recommended to treat with oseltamivir or zanamivir. (11) For Legionella, a urinary antigen test will be useful. (14) If SARS-CoV2 is suspected, a nucleic acid amplification test (NAAT) should be ordered. (18)
In patients with viral infections, clinicians must remain cautious of the development of bacterial superinfections, as secondary infection with S. aureus or S. pneumoniae has been linked with significant morbidity. (19)
References
- Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019; 200(7):e45–67.
- Pahal P, Rajasurya V, Sharma S. Typical Bacterial Pneumonia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 [cited 2021 Feb 11]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK534295/.
- Institut national d’excellence en santé et en services sociaux. Pneumonie acquise en communauté chez l’adulte [Internet]. 2017. Available from: https://www.inesss.qc.ca/fileadmin/doc/CDM/UsageOptimal/Guides-serieI/INESSS_Annexes_Rapport_GUO_PAC.pdf.
- Kaysin A, Viera AJ. Community-Acquired Pneumonia in Adults: Diagnosis and Management. AFP. 2016; 94(9):698–706.
- Gadkowski LB, Stout JE. Cavitary Pulmonary Disease. Clin Microbiol Rev. 2008; 21(2):305–33.
- Self WH, Courtney DM, McNaughton CD, Wunderink RG, Kline JA. High Discordance of Chest X-ray and CT for Detection of Pulmonary Opacities in ED Patients: Implications for Diagnosing Pneumonia. Am J Emerg Med. 2013; 31(2):401–5.
- Long L, Zhao H-T, Zhang Z-Y, Wang G-Y, Zhao H-L. Lung ultrasound for the diagnosis of pneumonia in adults. Medicine (Baltimore) [Internet]. 2017 [cited 2021 Feb 11]; 96(3). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5279077/.
- Torres A, Lee N, Cilloniz C, Vila J, Eerden MV der. Laboratory diagnosis of pneumonia in the molecular age. European Respiratory Journal. European Respiratory Society; 2016; 48(6):1764–78.
- Sattar SBA, Sharma S. Bacterial Pneumonia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 [cited 2021 Feb 11]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK513321/.
- Musher DM, Roig IL, Cazares G, Stager CE, Logan N, Safar H. Can an etiologic agent be identified in adults who are hospitalized for community-acquired pneumonia: results of a one-year study. J Infect. 2013; 67(1):11–8.
- Watkins RR, Lemonovich TL. Diagnosis and Management of Community-Acquired Pneumonia in Adults. AFP. 2011; 83(11):1299–306.
- Froes F. PSI, CURB-65, SMART-COP or SCAP? And the winner is... SMART DOCTORS. Pulmonol. Elsevier; 2013; 19(6):243–4.
- Kieninger AN, Lipsett PA. Hospital-Acquired Pneumonia: Pathophysiology, Diagnosis, and Treatment. Surgical Clinics of North America. 2009; 89(2):439–61.
- Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clinical Infectious Diseases. 2016; 63(5):e61–111.
- Gunasekera P, Gratrix A. Ventilator-associated pneumonia. BJA Education. 2016; 16(6):198–202.
- Gauer R. Early Recognition and Management of Sepsis in Adults: The First Six Hours. AFP. 2013; 88(1):44–53.
- Garvia V, Paul M. Empyema. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 [cited 2021 Feb 11]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK459237/.
- Kumar ST, Yassin A, Bhowmick T, Dixit D. Recommendations From the 2016 Guidelines for the Management of Adults With Hospital-Acquired or Ventilator-Associated Pneumonia. P T. 2017; 42(12):767–72.
- Hanson KE, Caliendo AM, Arias CA, Hayden MK, Englund JA, Lee MJ, et al. The Infectious Diseases Society of America Guidelines on the Diagnosis of COVID-19: Molecular Diagnostic Testing. Clinical Infectious Diseases [Internet]. 2021 [cited 2021 Feb 11]; (ciab048). Available from: https://doi.org/10.1093/cid/ciab048.
- Rynda-Apple A, Robinson KM, Alcorn JF. Influenza and Bacterial Superinfection: Illuminating the Immunologic Mechanisms of Disease. Infection and Immunity. American Society for Microbiology Journals; 2015; 83(10):3764–70.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.