Approach to
Acute Vision Loss
Sangeetha Santhakumaran1
Published online: 2 April 2021
1McGill University, Montreal, QC, Canada
Corresponding Author: Sangeetha Santhakumaran, email sangeetha.santhakumaran@mail.mcgill.ca
DOI: 10.26443/mjm.v19i1.492
Abstract
Acute vision loss is the temporary reduction of visual acuity or visual field, lasting from a few minutes to a few days. The etiologies of acute vision loss may be divided into anterior segment disease, retinal disease, optic nerve disease, or neurovascular disease. It is recommended to refer all presentations of acute vision loss for ophthalmologic consultation; however, the primary care physician plays an important role in determining the urgency of referral. The following article describes an approach to narrowing the differential diagnosis of acute vision loss, using relevant ocular history and physical exam findings. The features of common eye disorders relating to acute vision loss and their treatments are also discussed.
Tags: Vision loss, Amaurosis fugax, Retinal vascular occlusion
Question
A 69-year old man presents to your office with a 5-day history of sudden, transient episodes of left-eye vision loss. He describes the vision loss as a curtain being pulled over his eye, with each episode lasting approximately 20 minutes. The patient denies ocular pain, discharge, change in color vision, or photopsia (flashes of light). He also denies involvement of the right eye.
His past medical history is significant for hypertension and hypercholesterolemia, which is poorly controlled using perindopril and atorvastatin. He has no history of ocular trauma or ocular surgery. Upon examination, both eyelids and surrounding structures are unremarkable. There is an absence of conjunctival hyperemia or corneal opacity bilaterally. On examination, best-corrected visual acuity is 20/20 in the right eye (OD) and hand motion in the left eye (OS). Confrontational visual field testing reveals a full visual field OD, but an inability to detect movement in any quadrant OS. Extraocular motility is normal bilaterally in all directions. Penlight examination reveals absent pupillary constriction with direct light OS, but the consensual response is normal. The swinging flashlight test reveals a left relative afferent pupillary defect. Funduscopic exam reveals a diffusely opaque retina, apart from a small red spot at the location of the macula. There is generalized vascular narrowing, and pallor of the optic disc without swelling is noted.
Which condition is most consistent with the clinical presentation?
- Retinal detachment
- Retrobulbar optic neuritis
- Ischemic optic neuropathy
- Central retinal artery occlusion
- Central retinal vein occlusion
Answer
D. The sudden episodes of painless vision loss, history of hypertension and hyperlipidemia, and the funduscopic findings suggest central retinal artery occlusion (CRAO). The absence of photopsia makes the diagnosis of retinal detachment less likely. Optic neuritis is an unlikely cause as ocular pain and change in color vision were absent. Ischemic optic neuropathy typically presents with optic disc pallor, swelling, and splinter hemorrhages; the latter two findings were not present in this case. Central retinal vein occlusion also presents with optic disc swelling, venous engorgement, cotton-wool spots (due to the accumulation of axoplasmic material), and diffuse hemorrhages throughout the retina. Funduscopic findings characteristic of CRAO include the narrowing of arterial blood vessels and segmental blood flow, termed “boxcarring”. There is subsequent pallor of the optic disc and retina, with the exception of a “cherry red spot” in the macular region which reveals the underlying choroidal circulation.
Initial Approach
Acute vision loss is the temporary reduction of visual acuity or visual field, developing over a few minutes to a few days. (1) This symptom can be worrisome for many patients, and evaluation by an ophthalmologist is warranted to prevent permanent vision loss. (2) The role of the primary care physician is to determine whether the acute vision loss requires emergent, urgent, or non-urgent care.
Obtaining a comprehensive past medical history can help delineate a potential etiology. An initial characteristic to elicit is whether there is unilateral or bilateral eye involvement. Unilateral involvement suggests an ocular pathology whereas bilateral eye involvement suggests a neurologic etiology. Next, the physician should identify whether the vision loss is transient or persistent. Transient vision loss lasts less than 24 hours. The patient may describe the vision loss as blurry, indicative of a media-related ocular issue; dimming of vision, indicative of a vascular-related issue; or a reduction in visual field, suggesting an optic disc or neurologic issue. Associated flashes of light are suggestive of retinal detachment. Ocular pain and photophobia are usually present in corneal pathologies. Pain specifically on ocular movement is suggestive of, retrobulbar optic neuritis. Severe pain accompanied by tearing, nausea, and vomiting, is usually indicative of acute angle-closure glaucoma (AACG).
Visual acuity and visual fields should be assessed to confirm extent of vision loss. Additionally, pupillary reaction can be an important indicator of neurologic function. The swinging-flashlight test evaluates direct and consensual pupillary reflexes and may reveal a relative afferent pupillary defect (RAPD), indicative of monocular optic nerve disease. (2) Fundus examination of the retina may reveal retinal hemorrhaging, retinal whitening, cotton-wool spots (indicative of vascular disease), arteriolar narrowing, tortuosity, or venous engorgement. (3, 4, p. 56) The fundus exam may also reveal optic disc swelling, pallor, or an increase in the cup-to-disc ratio. The remainder of the physical exam may be tailored based on suspicion of cardiovascular, neurologic, or other disease.
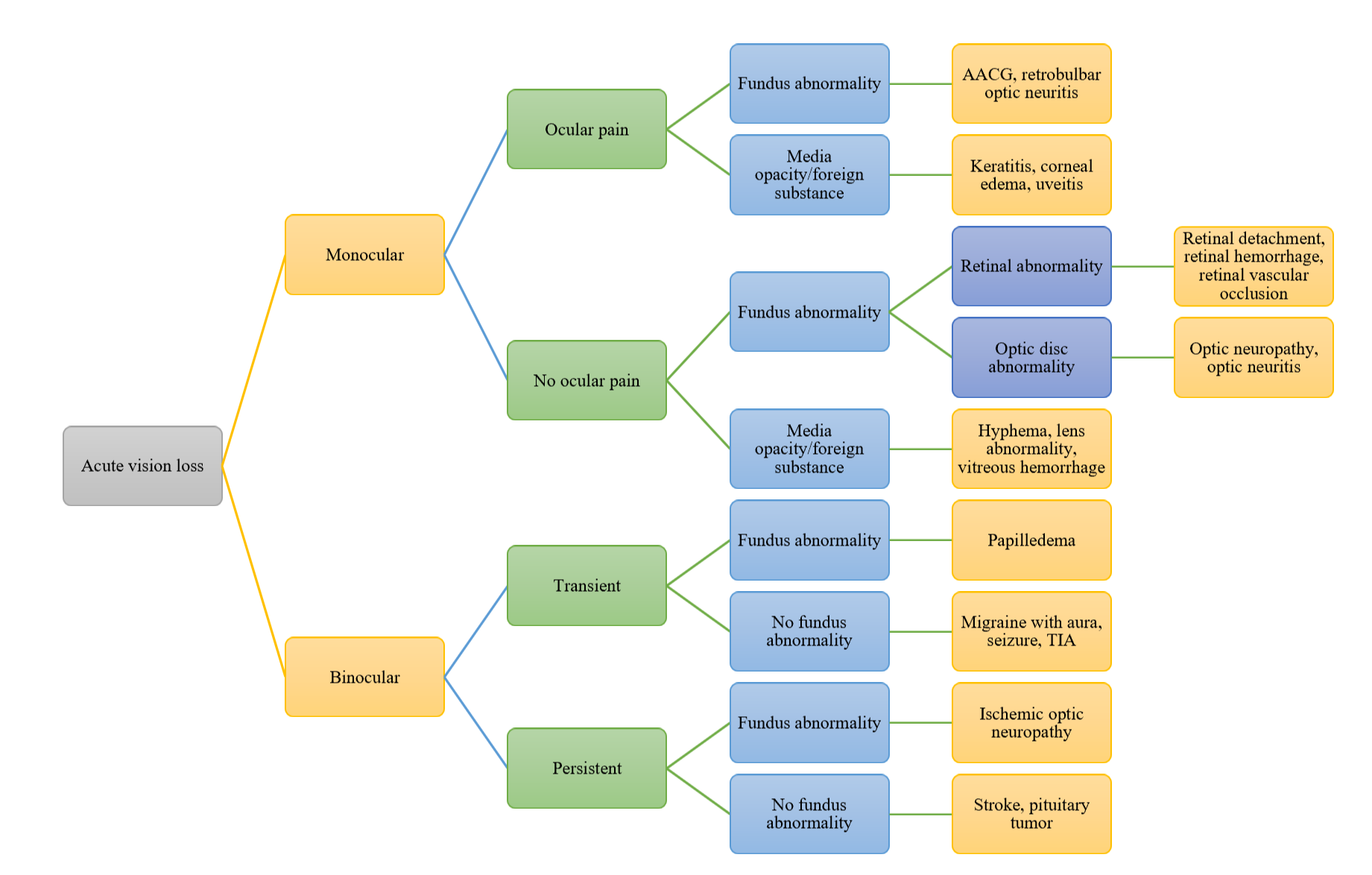
AACG: acute angle-closure glaucoma, TIA: transient ischemic attack
Adapted from (6) and (7)
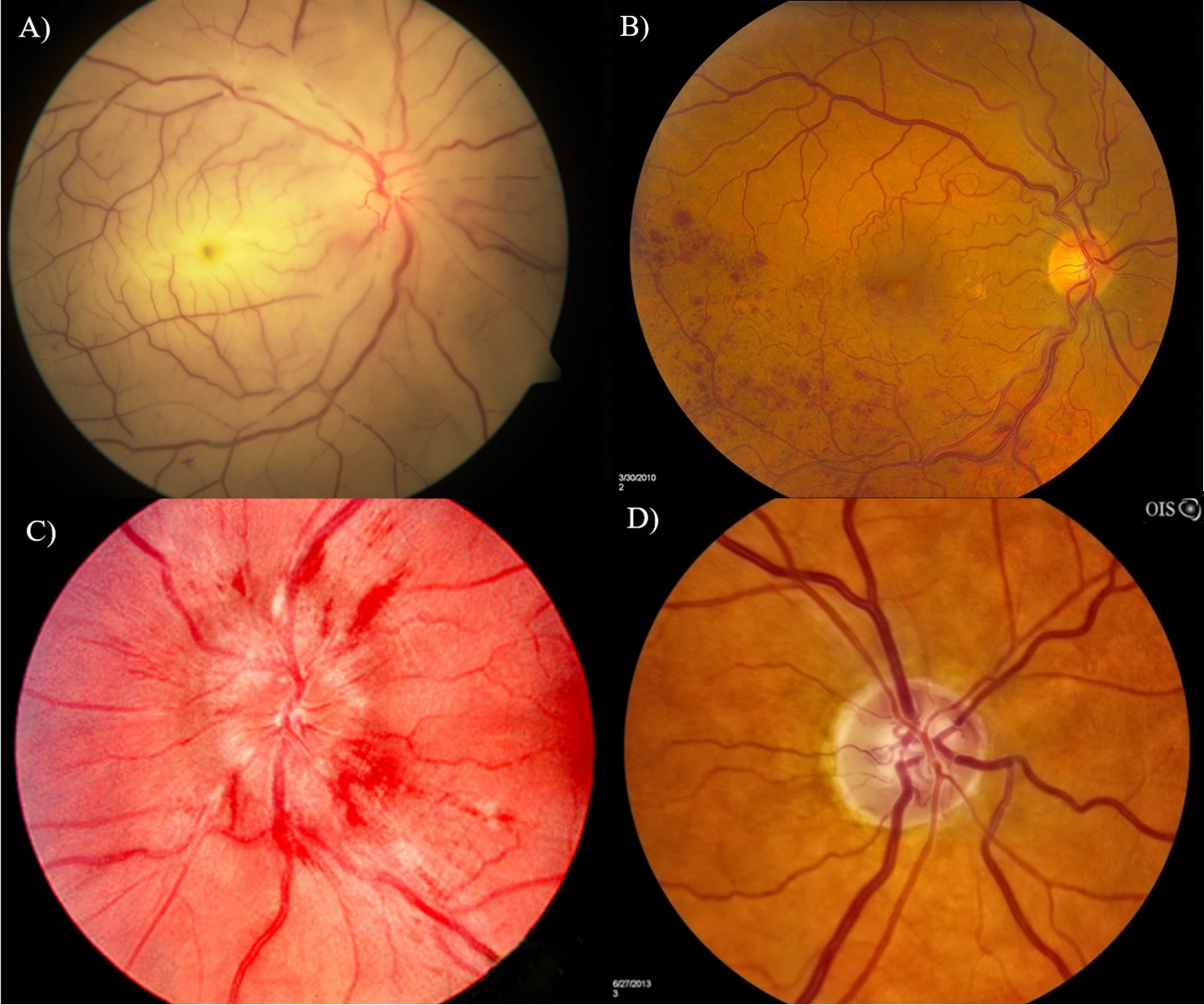
A) Central retinal artery occlusion, image obtained from (17)
B) Branch retinal vein occlusion, image obtained from (18)
C) Papilledema, image obtained from (19)
D) Glaucoma, image obtained from (20)
Beyond the Initial Approach
Diseases that present with acute vision loss can be divided into monocular and binocular involvement. Of monocular diseases, the presence of ocular pain is generally indicative of an optical media or fundus abnormality. The anterior segment plays an important role in light refraction; therefore, pathology in this region may lead to blurry vision. Keratitis refers to corneal inflammation, which may occur due to infection, injury, or allergy. (1) On examination, clouding of the cornea and severe irritation are characteristic. (1) Corneal staining may be used to evaluate epithelial defects. Uveitis refers to inflammation of the iris, ciliary body, and/or choroid. (7) Uveitis may present with ocular pain and redness, and photophobia if the iris is involved. (7) Both anterior and posterior uveitis may occur due to infection; however, anterior uveitis is also associated with systemic disease. (7) The mainstay of treatment for anterior segment inflammation is topical steroids, mydriatic eyedrops, and topical or oral antimicrobial agents where appropriate. (7)
AACG is a painful eye disease that occurs as aqueous fluid is insufficiently drained, leading to increased intraocular pressure and subsequent optic nerve damage. (14) Symptoms include vision loss, eye pain and headache, nausea/vomiting, and seeing halos around lights. (5, 14, 15) Signs include a fixed, mid-dilated pupil, a closed anterior chamber angle upon slit-lamp examination, and optic disc pallor and cupping (cup-to-disc ratio of 0.6 or greater). (5) Tonometry demonstrates an increased intraocular pressure ranging from 40 to 80mmHg. (1) Treatment is focused on the reduction of intraocular pressure, aqueous fluid production, and inflammatory damage. (15) Laser peripheral iridotomy may relieve anterior chamber blockage after the acute attack is resolved. (15)
Painless monocular disease may also be divided into pathologies of the media or fundus. Fundus involvement may be further subdivided into retinal or optic disc abnormalities. Visual field defects generally suggest a retinal or neurologic pathology. Retinal vascular occlusion should be suspected in a patient with cardiovascular disease. (5) Funduscopic examination can pinpoint the subtype and extent of vascular occlusion. Further evaluation with optical coherence tomography and fluorescein angiography may assist with clinical decision making. Central retinal artery occlusion is an ocular emergency in which fleeting vision loss occurs, termed amaurosis fugax. (8) RAPD may be seen on examination. Initially, fundoscopy shows arterial narrowing and segmental blood flow (boxcarring). (3) After several hours, the fundus appears opaque apart from a “cherry-red” spot in the macular region. (8) The most common cause of CRAO is carotid atherosclerosis, seen on carotid artery imaging. (9) Immediate treatment is warranted and involves ocular massage, paracentesis and IV acetazolamide to reduce intraocular pressure, carbogen inhalation to induce vasodilation, and laser embolectomy for clot lysis. (1) Central retinal vein occlusion is an urgent event presenting similarly to CRAO, in which venous engorgement occurs. However, funduscopic examination shows optic disc swelling, diffuse retinal hemorrhage, and cotton-wool spots which are representative of the axoplasmic material. (3) Branch artery and branch retinal vein occlusion may produce partial vision loss, but if central vision is not affected, they may also go unnoticed. (8) Retinal detachment is a non-vascular retinal pathology that may result in acute vision loss, due to oxygen and nutrient-deprived retinal tissue. (1) Symptoms include floaters, photopsia, and visual field loss. (1) Funduscopic examination may reveal dulling of the red reflex and an elevated portion of the retina. (1) Retinal imaging with ocular sonography and indirect ophthalmoscopy can be used to further evaluate the peripheral retina. (2) Ophthalmologic treatment should be sought immediately and includes pneumatic retinopexy, scleral buckling, and vitrectomy. (10) Optic neuritis refers to optic nerve inflammation, and is most commonly caused by multiple sclerosis, but may also occur due to infection or autoimmune disease. (13) Symptoms include loss of red-green color discrimination, pain with eye movement, and temporary vision loss. (1) A RAPD is typically present. (1) Funduscopic examination may reveal a swollen optic disc; however, retrobulbar optic neuritis often results in a normal fundus exam. (13) Vision loss often recovers completely without treatment, but steroid treatment may be used in refractory cases. (13)
Causes of binocular vision loss may be subdivided into transient and persistent vision loss. Similar to monocular diseases, the transient and persistent binocular diseases may be further subcategorized based on fundus involvement. Papilledema refers to the non-painful swelling of bilateral optic nerves seen on fundoscopy, occurring due to increased intracranial pressure. (9) Symptoms include mild persistent blurred vision or visual disturbances that alter with change in position, headache, and nausea/vomiting. (9) Papilledema is differentiated from optic neuritis with normal pupillary reflexes and bilateral presentation. (1) Neuroimaging may pinpoint the cause of increased intracranial pressure, such as a mass or hemorrhage. (9) If no fundus abnormality is present, the possibility of migraine, seizure, or transient ischemic attack (TIA) should be considered. Migraines may present with a temporary loss of vision lasting several minutes, with photopsias/scintillations progressively worsening as the headache worsens. (6) Conversely, the visual obscurations seen in seizures are typically maximal at onset. (9) There may be multiple episodes of vision loss relating to the recurrence of migraines or seizures. In the setting of a stroke, the visual field is affected if the occipital lobe is involved. (9) In a transient ischemic attack, the ocular symptoms disappear within 24 hours. In a stroke, however, vision loss may be permanent. (6)
If binocular vision loss persists for greater than 24 hours, ischemic optic neuropathy should be considered. Giant cell arteritis is a form of vasculitis affecting elderly individuals, commonly involving branches of the carotid artery. (9) Symptoms include a temporal headache and jaw claudication. (11) A potentially devastating complication is arteritic-anterior ischemic optic neuropathy (AAION), where blood flow to the optic nerve is interrupted and visual field loss occurs. (11) A temporal artery biopsy confirms the diagnosis. (10) Corticosteroid therapy is provided immediately to prevent permanent vision loss. (5) Non-arteritic anterior ischemic optic neuropathy (NAION) may also result in the blurring or loss of vision. (11) Systemic risk factors include hypertension, diabetes mellitus, and hyperlipidemia. (12) There is no specific treatment for NAION. (12)
In the absence of fundus abnormality with persistent vision loss, a lesion further than the optic disc should be considered. As the optic nerve travels towards the brain, a portion of the nerve fibres responsible for temporal vision decussate, forming the optic chiasm. A lesion in this area, caused by a disease process such as a pituitary tumor, may result in bitemporal hemianopia. (6, 9) Post-chiasmic (optic tract) lesions present with vision loss in one side of the visual field, termed homonymous hemianopia. (2) This may occur due to a stroke, infection, or surgery. (6)
Of the aforementioned diseases, the more common presentations of acute vision loss include cornea-related pathologies, retinal vascular occlusion, and trauma. (2, 7) Although all etiologies of acute vision loss require ophthalmological referral, the following conditions warrant emergent care: acute central retinal artery occlusion, ischemic optic neuropathy, AACG, and suspected cerebral vascular accidents. (6)
References
- Leveque T. Approach to the adult with acute persistent visual loss. In: Trobe J, editor. UpToDate. Waltham, MA: Wolters Kluwer; 2020.
- Acute Vision Loss [Internet]. Merck Sharp & Dohme Corp. 2019. Available from: https://www.merckmanuals.com/en-ca/professional/eye-disorders/symptoms-of-ophthalmologic-disorders/acute-vision-loss#v951557.
- Sudden Visual Loss [Internet]. WebMD LLC. 2019 [cited November 1, 2020]. Available from: https://emedicine.medscape.com/article/1216594-overview.
- Harper RA. Basic ophthalmology. Ninth edition. ed. San Francisco, CA: American Academy of Ophthalmology; 2010.
- Prasad S, Galetta SL. Approach to the patient with acute monocular visual loss. Neurol Clin Pract. 2012;2(1):14-23.
- Pelletier AL, Thomas J, Shaw FR. Vision loss in older persons. Am Fam Physician. 2009;79(11):963-70.
- SooHoo JR. Evaluation of Vision Loss. 2018. In: BMJ Best Practice [Internet]. London, UK: BMJ Publishing Group. Available from: https://bestpractice.bmj.com/topics/en-us/960.
- Duplechain A, Conrady CD, Patel BC, Baker S. Uveitis. StatPearls [Internet]. 2020.
- Haymore JG, Mejico LJ. Retinal Vascular Occlusion Syndromes. International Ophthalmology Clinics. 2009;49(3):63-79. 0
- Hahn P, Fekrat S. Best practices for treatment of retinal vein occlusion. Current Opinion in Ophthalmology. 2012;23(3):175-81.
- Kale N, Eggenberger E. Diagnosis and management of giant cell arteritis: a review. Current Opinion in Ophthalmology. 2010;21(6):417-22.
- Miller NR. Current Concepts in the Diagnosis, Pathogenesis, and Management of Nonarteritic Anterior Ischemic Optic Neuropathy. Journal of Neuro-Ophthalmology. 2011;31(2):e1-e3.
- Toosy AT, Mason DF, Miller DH. Optic neuritis. The Lancet Neurology. 2014;13(1):83-99.
- Wright C, Tawfik MA, Waisbourd M, Katz LJ. Primary angle‐closure glaucoma: an update. Acta ophthalmologica. 2016;94(3):217-25.
- Prum BE, Herndon LW, Moroi SE, Mansberger SL, Stein JD, Lim MC, et al. Primary angle closure preferred practice Pattern® guidelines. Ophthalmology. 2016;123(1):P1-P40.
- Givre S, Stavern GPV. Amaurosis fugax (transient monocular or binocular visual loss). In: Brazis PW, Trobe J, editors. UpToDate. Waltham, MA: Wolters Kluwer; 2019.
- Kwak H-W. Central Retinal Artery Occlusion. In: Occlusion CRA, editor. Retina Image Bank: American Society of Retina Specialists; 2012.
- Calahoun JS. Branch Retinal Vein Occlusion [photograph]. Jacksonville (FL): American Society of Retina Specialists; 2013. 1 photograph: color.
- Trobe J. Papilledema. In: Papilledema, editor. Wikimedia Commons. Ann Arbor, Michigan: Wikimedia; 2011.
- Calahoun JS. Normotension Glaucoma. In: Glaucoma N, editor. Retina Image Bank. Florida, USA: American Society of Retina Specialists; 2013.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.