Brief Report
Assessing the appropriateness of colorectal cancer screening in very elderly women: A cross-sectional analysis
Jérôme Williams1, Zhou Fang1, Roland Grad1
Published online: 3 March 2021
1McGill University, Montreal, QC, Canada
Corresponding Author: Jérôme Williams, email jerome.williams@mail.mcgill.ca
DOI: 10.26443/mjm.v19i1.339
Abstract
The Canadian Task Force on Preventive Health Care recommends against screening for colorectal cancer after age 75. This recommendation is based in part on lag time to mortality benefit and a reduced life expectancy in the very elderly. To explore the extent to which screening for colorectal cancer is appropriately ordered in primary care, we performed a cross-sectional study in women aged 80-84 at an academic family medicine clinic in Montreal. Appropriateness was assessed using a validated life expectancy calculator, with a 10-year life expectancy of >50% serving as the threshold for appropriateness. Among women 80-84 years of age under the care of a physician in 2016 (N=144), 95 fecal immunochemical tests were ordered from 2016-2019. Of these, 41 were screening tests, and 16/41 (39%; 95% CI 24% to 54%) were deemed to be inappropriate. This finding suggests a need to improve screening decisions for elderly women followed in primary care.
Tags: overscreening, colorectal cancer, low-value care, quality improvement, choosing wisely
Introduction
Screening is used to identify unrecognized disease in asymptomatic, seemingly healthy patients. In making decisions about cancer screening in clinical practice, determining the probability of benefit and harm is difficult. Hence, many physicians follow recommendations from clinical practice guidelines, such as those from the Canadian Task Force on Preventive Health Care (CTFPHC). When screening falls outside the recommendations of such guidelines and occurs in the absence of high-quality evidence, physicians run the risk of overscreening their patients. Overscreening refers to the use of a screening test at ages younger or older than the range recommended by national guidelines, or at a greater frequency than recommended. This can be harmful to patients and increases costs to the health care system. Awareness of overscreening is increasing, due in part to organizations such as Choosing Wisely Canada, which operates as the national voice for avoiding unnecessary medical tests.
Colorectal cancer is a leading cause of mortality, but despite a rising incidence of colon cancer with increasing age, the CTFPHC recommends against screening for it after the age of 75. (1) This weak recommendation is based on reduced life expectancy (LE) in the very elderly, the long time lag needed for any mortality benefit from screening, and the harms associated with invasive follow-up diagnostic tests and treatments. (2) On balance, when screening offers a greater probability of harm than benefit, it should not be offered. Evidence suggests a LE of less than 10 years represents a reasonable threshold for suspending screening for colorectal cancer. (3) Specialty groups such as the Canadian Association of General Surgeons endorse this 10-year LE threshold. (4) In this study, we sought to assess the extent of fecal immunochemical test (FIT) overscreening for colorectal cancer in women aged 80-84 in primary care.
Methods
We performed a cross-sectional analysis of data obtained from the electronic medical records of an academic family medicine center in Montreal. Ethics approval was granted by the Research Ethics Committee of the CIUSSS West-Central Montreal.
We identified all women aged 80-84 who were followed at the center by a family physician. Since men and women have different average LEs at any given age, males were excluded to keep the number of chart reviews to a manageable number. Furthermore, to our knowledge, there is no evidence of a sex or gender bias in screening for colorectal cancer. The age range of 80-84 was chosen because at 80 years of age, Canadian women have a median LE of 10.1 years. Thus, 80 represents the age at which screening decisions based on a 10-year LE are challenging given roughly equal probabilities of a LE less or greater than 10 years.
We filtered our total patient list by selecting women referred for a FIT from January 2016 to December 2019. FIT is the screening test presently used in Quebec for colorectal cancer screening in average risk populations.
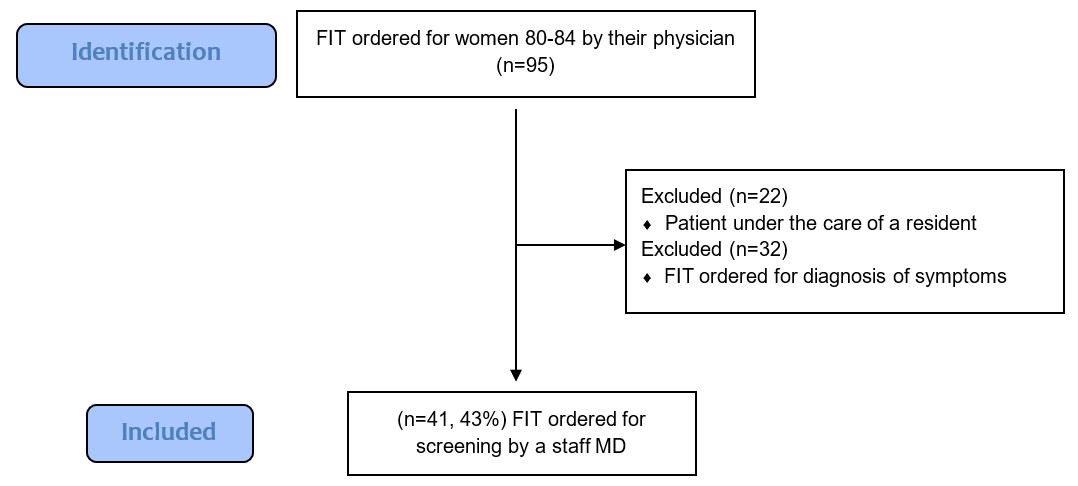
Each patient record was independently examined by two reviewers (ZF, JW). First, all women whose FIT was ordered by a resident physician were excluded to avoid a possible bias related to test ordering decisions made by trainees. Second, we excluded cases where FIT was ordered for diagnostic purposes, such as patients with gastrointestinal symptoms or anemia. The senior author reviewed cases where the reason for ordering the test was unclear.
We assessed patient LE at the time of ordering the FIT using an online calculator to determine the appropriateness of screening of each patient in our cohort. (5) This calculator was based on the Charlson Comorbidity Index, a validated method of predicting the probability of 10-year mortality. (6) All comorbidities weighted in this calculator were considered, and a LE prediction for each patient was recorded. We considered FITs to have been inappropriately ordered for patients whose 10-year LEs were less than 50%. A 95% confidence interval (CI) was calculated using the normal approximation method.
Results
A total of 144 women aged 80-84 were registered at the clinic in 2016. Between 2016-2019, 95 FITs were ordered among 80 women. Eleven women received two tests over this period, and two women received three. Of the 95 FITs, 22 were excluded because they were ordered by a resident physician. An additional 32 FITs were excluded because they were ordered for diagnostic purposes. Forty-one FITs were ordered as screening tests by attending physicians for 41 different women (Figure 1).
Of these 41 cases, 10-year LE estimates for individual patients ranged from 2% to 53%. Sixteen of these 41 tests were ordered in patients with a 10-year LE of less than 50%. The percentage of inappropriate FIT testing was therefore 39% (95% CI 24% to 54%). It is worthwhile to note that no women received more than one inappropriate test.
Discussion
We found that, according to current best practice, approximately 40% of FIT screening tests ordered for women between the ages of 80-84 were inappropriate. Taking the lower bound of the 95% CI as a conservative estimate, one quarter of screening FITs confer more harm than benefit. Because this study was based in a single center, the findings may not generalize elsewhere. However, our findings reinforce the notion that there is room to reduce unnecessary care in Canada. (7).
Overscreening cannot be ignored given the burden it places on our publicly funded health system, and on individuals. With regard to the former, when scaled to an entire province, overscreening represents a waste of limited healthcare resources. In Alberta, 1.7% of seniors over the age of 75 received an inappropriate colorectal cancer screening test at least once in a 3-year period (2012-2015). (8) At a cost of $669 per person, these 4,035 tests amounted to a cost of $269,415. As Quebec has twice the population of Alberta, significant cost savings may be possible if colorectal cancer overscreening is reduced. With respect to patients, overscreening is not merely a waste of their time. The most serious harm from overscreening is the avoidable anxiety and unnecessary invasive follow-up that arises when a screening test produces a false positive result.
Reducing overscreening will likely require a multifaceted approach, as many factors influence physician decision-making. Further education on how screening guidelines are constructed, and on the underlying logic of using LE in screening decisions, may represent an important start. Schoenborn et al. found that even if physicians appreciate the problem of overscreening, some are skeptical of applying population-level guidelines to individual patients, which appears to be due to a misunderstanding of the epidemiological basis for these recommendations. (9) Confronting the action bias that afflicts both patients and their physicians will also be of critical importance. (10)
In conclusion, we see a need to improve colorectal cancer screening decisions for women aged 80-84 in primary care in Quebec.
References
- Canadian Task Force on Preventive Health Care. Recommendations on screening for colorectal cancer in primary care. CMAJ. 2016 Mar 15;188(5):340-8.
- Lee SJ, Leipzig RM, Walter LC. "When Will it Help?" Incorporating Lagtime to Benefit into Prevention Decisions for Older Adults. JAMA. 2013 Dec 25;310(24):2609-10.
- Grad R, Thériault G, Singh H, Dickinson JA, Szafran O, Bell NR. Age to stop?: Appropriate screening in older patients. Can Fam Physician. 2019 Aug 1;65(8):543-8.
- The Canadian Association of General Surgeons (CAGS) has developed a list of 6 things physicians and patients should question in general surgery [Internet]. Choosing Wisely Canada. [cited 2020 Nov 1]. Available from: https://choosingwiselycanada.org/general-surgery/
- Charlson Comorbidity Index (CCI) [Internet]. MDCalc. [cited 2020 Oct 18]. Available from: https://www.mdcalc.com/charlson-comorbidity-index-cci
- Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data From 6 Countries. Am J Epidemiol. 2011 Mar 15;173(6):676-82.
- Gapanenko K, Lam D, Parker M, D'Silva J, Johnson T. Unnecessary Care in Canada. Healthc Q Tor Ont. 2017;20(3):10-1.
- McAlister FA, Lin M, Bakal J, Dean S. Frequency of low-value care in Alberta, Canada: a retrospective cohort study. BMJ Qual Saf. 2018;27(5):340-6.
- Schoenborn NL, Massare J, Park R, Pollack CE, Choi Y, Boyd CM. Clinician Perspectives on Overscreening for Cancer in Older Adults With Limited Life Expectancy. J Am Geriatr Soc. 2020;68(7):1462-8.
- Scott IA, Soon J, Elshaug AG, Lindner R. Countering cognitive biases in minimising low value care. Med J Aust. 2017 May 15;206(9):407-11.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.