Approach to
Febrile Seizures
Anita Dabirzadeh1
Published online: February 1, 2021
1McGill University, Montreal, QC, Canada
Corresponding Author: Anita Dabirzadeh, email anita.dabirzadeh@mail.mcgill.ca
DOI: 10.26443/mjm.v19i1.317
Abstract
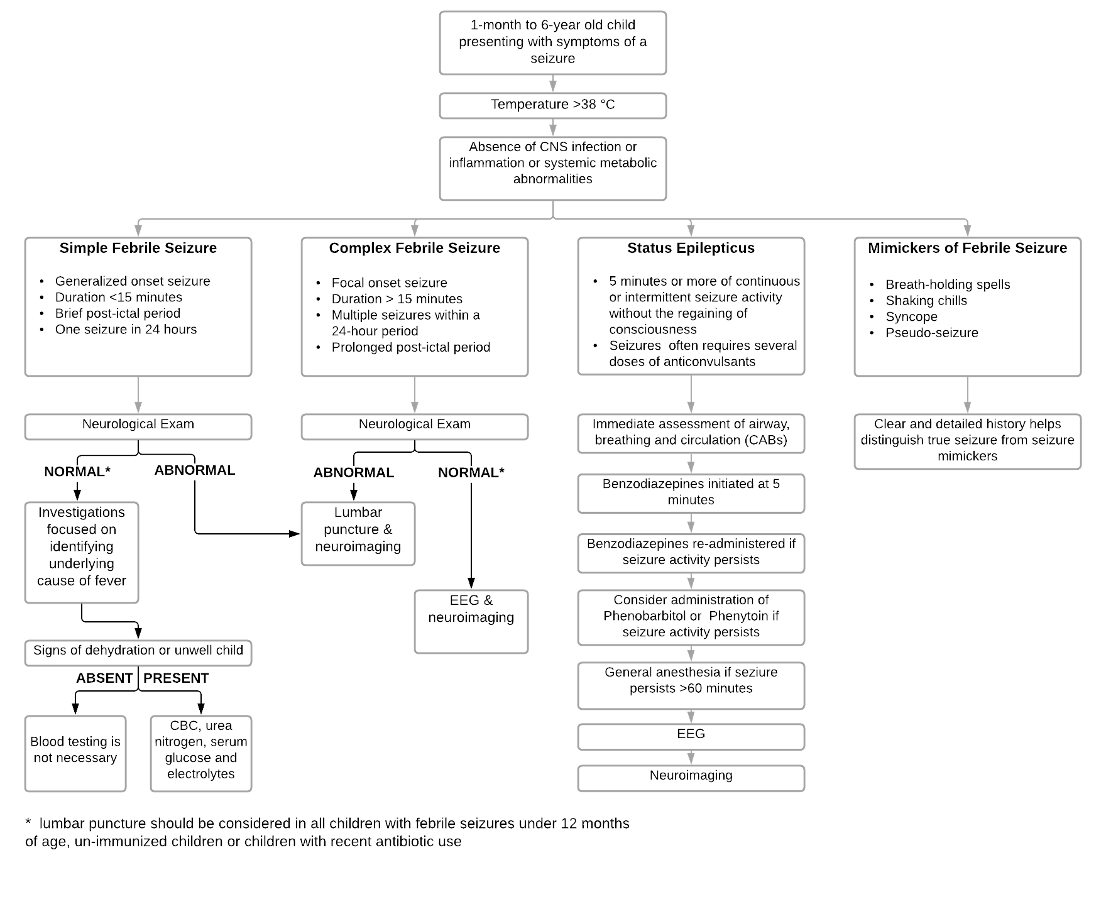
This approach article provides pre-clinical students and students preparing for rotations in pediatrics with an approach to the evaluation, diagnosis and management of patients with febrile seizures. Febrile seizures are the most common childhood neurological disorder. They are most commonly defined as a seizure occurring in a child 6-months to 6-years of age with a fever in the absence of an intracranial infection or other identifiable cause. The vulnerability of a child’s central nervous system to fever is thought to be responsible for febrile seizures. They can be categorized as either simple or complex, depending on seizure duration, characteristics and recurrence. This categorization directs the necessary diagnostic investigations. While the majority of febrile seizures are benign, students must learn to differentiate benign febrile seizures from other dangerous causes of seizure, such as a central nervous system infection, and identify the life-threatening condition of status epilepticus.
Tags: Pediatrics, Seizure, Neurology, Infectious Disease, Febrile Illness
Question
You are a third-year medical clerk working in the pediatric emergency room. Layla, an 18-month-old, presents with a history of a 3-minute seizure. After speaking to her parents, you find out that preceding the seizure, Layla had been experiencing a 12-hour history of gastrointestinal symptoms. Layla was born at 40 weeks via spontaneous vaginal delivery. Her mother’s maternal history was unremarkable and screening for group B strep at 37-weeks was negative. At birth, Layla weighed 3.9 kg (8.6 lb.) with APGAR scores of 7 and 9 at 1 and 5 minutes respectively. Layla has reached her developmental milestones at appropriate times with first words spoken at 8 months, crawling beginning at 9 months and walking at 13 months. Layla was breast-fed exclusively for 6 months before transitioning to formula feeds. She was introduced to solid foods at 9-months of age. Her growth charts indicate that she has been following the 85th percentile for weight and length. Layla has no previous medical history; no known allergies and all her immunizations are up to date. Layla currently lives with her mother and father who both work full time as secondary school teachers. Layla has been attending daycare since she was 6-months of age and her parents report that she enjoys her time there. Layla’s parents deny recent travel or exposure to sick contacts.
You observe the following findings on physical exam:
General Appearance: An irritable but alert infant with no signs of dehydration and normal capillary refill.
Vital Signs: HR: 110, RR: 26, BP: 90/50, Temp: 39.5 °C, O2 Sat: 98\% on room air
Growth Parameters: Weight: 13.4kg (85th percentile), Height/Length: 86cm (85th percentile), Head Circumference: 47cm (50th percentile)
Head: Fontanelle are soft and non-protruding.
ENT: Normal temporomandibular joints bilaterally, pharynx/palate normal
Neck: No cervical adenopathy, neck is supple, negative Kernig and Brudzinski signs
Respiratory: Good air entry bilaterally, no adventitious lung sounds
Cardiovascular: Normal S1, S2, no S3 or S4, no murmurs on auscultation, radial, brachial and femoral pulses normal, no signs of cyanosis, normal capillary refill
Abdomen: No scars, abdomen soft and non-distended, no organomegaly, no tenderness or guarding, no palpable mass
Neurological: Pupils equal and reactive, extraocular movements intact, no facial asymmetry, normal tone and reflexes, moving all limbs symmetrically, normal gait, normal cerebellar exam
Which one of the following investigations are indicated in the acute management of Layla?
- Lumbar puncture
- EEG
- Brain MRI
- CBC, serum glucose, urea nitrogen and electrolytes
- No further investigations are needed, provide reassurance to parents
Answer
E. From the history that has been gathered from Layla’s parents, it appears that she had a simple febrile seizure as a result of a recent gastrointestinal illness. As Layla’s vitals, neurological exam and general physical exam are normal apart from fever, no specific diagnostic workup is required. As Layla’s neurological exam was normal, intracranial infection or underlying structural mass is unlikely. As a result, lumbar puncture is not warranted. As she is not exhibiting any signs of dehydration and is generally appearing well, CBC, serum glucose, urea nitrogen and electrolytes should not be routinely ordered. Furthermore, MRI and EEG are not routinely recommended in the evaluation of children with simple febrile seizures. Since Layla appears wells, her management includes discharge and close follow-up with her primary care physician as needed.
Initial Approach
Febrile seizures are the most common neurological condition of childhood. Approximately 3-4\% of children in North America will experience an episode prior to the age of 5. (1) Febrile seizures are defined as seizures occurring in childhood after one month of age, associated with febrile illness without any evidence of intracranial infection or other identifiable cause. Febrile seizures most commonly occur between 6-months to 6-years of age. (1)
Clinical Presentation
A thorough medical history and examination is crucial in the evaluation of a child with a suspected febrile seizure. (2) Key elements include description of the onset, duration and characteristics of the episode. Examples include loss of consciousness, foaming at the mouth, tongue biting, difficulty breathing, cyanosis, and rhythmic repetitive movements of both arms and legs. (2,3) These details will help distinguish true seizures from seizure mimickers. Elements that are suggestive of seizure activity include unresponsiveness, tongue biting, lip smacking, rolling back of the eyeballs and flickering eyelids. (3) Mimickers of seizure include breath-holding spells, rigors, pseudo-seizures and syncope. Breath holding spells are often triggered by emotional distress or pain and can be distinguished from seizure activity. (4) Rigors are not typically associated with a loss of consciousness. (2) Although syncope may be associated with muscular twitching events, there is usually a prodrome of pallor and perspiration, which distinguishes it from a seizure. (4)
Past Medical History, Physical Exam and Red Flags
It is important that the child’s caregivers provide a history of recent respiratory or gastro-intestinal illness. It is also important to ask caregivers about recent vaccinations or medication use such as antibiotics. The majority of children who experience a febrile seizure experience it on their first day of illness. However, a febrile seizure may also be the first indication of infection. (3) A complete general physical exam should be done to identify the underlying cause of fever. Furthermore, it is vital to ascertain a history of red flags from caregivers as these will alter the management of the child. Red flags in a child presenting with febrile seizure include a history of developmental delay, lethargy or head injury. A complete neurological examination of the child is also necessary to identify red flags associated with an acute neurological problem such as central nervous system infection. (5) Red flags suggestive of meningitis include irritability, altered level of consciousness, positive Brudzinski and Kernig’s signs, neck stiffness, photophobia, petechial rash, hypotension and bulging fontanelles. (3)
Classifications
Febrile seizures can be categorized as either simple or complex depending on seizure duration, characteristics and recurrence. The type of seizure a child experienced will dictate how the condition of the child is managed. Simple febrile seizures account for approximately 80\% of all febrile seizures. (1) They are typically generalized and associated with tonic-clonic jerking of bilateral limbs that last between several seconds to 15 minutes. (2) On presentation, a child with a simple febrile seizure is typically alert as post-ictal symptoms generally resolve within 10-15 minutes. Simple febrile seizures should not reoccur within a 24-hour period. In contrast, complex febrile seizures are often focal, last longer than 15-minutes, may reoccur more than once in a 24-hour period and are associated with a prolonged period of post-ictal drowsiness or hemi-paresis known as Todd’s Palsy. (2) Status epilepticus is the most serious form of febrile seizure and is defined as 5 minutes or more of continuous or intermittent seizure activity without the regaining of consciousness between seizures. Prolonged seizure activity, typically defined as longer than 30 minutes, can cause neuronal injury and death. (6)
Investigations
Diagnostic investigations for a child experiencing a febrile seizure is dependent on whether the seizure was simple, complex or status epilepticus. In cases of simple febrile seizure with normal neurological exam findings, no further investigations are necessary. (5) Evaluations should instead focus on identifying the underlying cause of fever. (2) A complete blood cell count, urea nitrogen, serum glucose and electrolytes should be considered in children with a history of vomiting or diarrhea or if signs of dehydration are present. (2) While a lumbar puncture is not necessary for well-appearing children after a simple febrile seizure, it is recommended for children under the age of 12-months as physical exam signs of meningitis are extremely subtle in this age group. (5) Lumbar puncture with cell counts, gram stain and culture, protein and glucose should also be performed in a child with concerning neurological examination findings as CNS infection must be ruled out. (5) Furthermore, lumbar puncture should be considered in un-immunized children or children with recent antibiotic use as this increases suspicion of an underlying bacterial infection. (2) It is important to note, however, that in a child with a neurological exam suggestive of a space-occupying lesion, neuroimaging must be immediately performed and lumbar puncture is contraindicated due to suspected increased intracranial pressure. (7) Electroencephalography (EEG) is of limited value and therefore not recommended in children with a first presentation simple febrile seizure. (5)
Children presenting with complex febrile seizures warrant further evaluation to identify any potential structural or metabolic causes, particularly if this is their first episode. EEG is indicated in the evaluation of a complex febrile seizure as there is a risk of an underlying epileptic syndrome. (1) Neuroimaging with MRI or CT should be considered in children with neurological abnormalities on physical exam, history of head injury, signs of increased intracranial pressure or suspected intracranial abnormality. (3)
Management
Children presenting in status epilepticus require immediate resuscitative efforts. (8) It is critical that the child’s airway is maintained, supplemental oxygen is provided, and cardiac monitoring is established (CABs). (6) Administration of benzodiazepines to terminate seizure activity is a priority five minutes after seizure onset. (6) As intravenous access in an actively seizing child may be difficult, benzodiazepines may be administered rectally, intranasally, buccally or intramuscularly. It is important to recognize that some patients require further doses of benzodiazepines. Status epilepticus is a life-threatening emergency situation which rarely stops spontaneously and often requires several doses of anticonvulsants to control. (2) Children with status epilepticus require an extended period of observation as seizure activity may recur. Long-term management of patients should include EEG and neuroimaging.
Beyond the Initial Approach
Risks of Recurrence and Epilepsy
The etiology of febrile seizures is not fully understood and likely thought to be multifactorial. Theories suggest that febrile seizures may be due to the vulnerability of the developing child’s central nervous system to the effects of fever in combination with genetic factors. (3) Identified risk factors for febrile seizure include age, prematurity, developmental delay, viral infection, daycare attendance, prenatal exposure to nicotine and/or alcohol and a family history of seizures. (3,17) Furthermore, no single causative gene has been identified, although a familial association has been demonstrated as the risk of febrile seizure is 25\% if one sibling is affected and 33\% if both parents or more than one sibling is affected. (11) Recurrence of febrile seizures in the future is also relatively common with approximately 33\% of children having a second febrile seizure during early childhood. (12) Seventy percent of reoccurrences occur within the first year following a febrile seizure and 90\% within 2 years. (12) Risk factors for recurrent febrile seizures include first seizure occurring prior to 18 months of age, family history of febrile seizure, seizure associated with a fever below 39 degrees. (12) Furthermore, children experiencing a simple febrile seizure have a 1\% risk of developing epilepsy compared to the 0.5\% incidence in the general population. (15) Children with a complex febrile seizure have a 4-6\% risk of future epilepsy. (3,16) Risk factors for the development of epilepsy include previous neurodevelopmental impairment, family history of epilepsy and complex febrile seizures.
Caregiver Counselling
A febrile seizure can be an extremely frightening experience for caregivers, particularly if the seizure is prolonged. Parents may be terrified that their child will experience long-term brain damage as a result of their seizure or have epileptic syndrome. It is important to reassure caregivers that the majority of febrile seizures are harmless and are not associated with complications of long-term brain damage or intellectual disability. (13) Caregivers should be informed that their child may experience another febrile seizure in the future and be counselled on steps they can take to ensure their child’s safety. This includes placing the child on their side to prevent aspiration, removing or loosening tight-fighting clothing, ensuring that the child is on a soft surface with all nearby objects removed and tracking the length of the seizure. (12) Parents should also be instructed to call emergency medical services should a recurrent seizure last longer than five minutes, if the child looks cyanotic or appears to have difficulty breathing, if the seizure is focal or if the child experiences a second seizure within 24 hours. While febrile seizures occur as a result of a fever, the rapidity of fever onset has not been found to be associated with an increased risk of seizure.
As such, antipyretics should not be given as they have not been shown to reduce the risk of febrile seizure prophylactically. (9,10) While the majority of febrile seizures are harmless, children that experience recurrent febrile seizures are at an increased risk of delayed language and memory development. (14) Caregivers of children with recurrent febrile seizures should therefore be informed so that adequate developmental support can be put in place.
References
- Leung AKC, Robson WLM. Febrile Seizures. J Pediatr Heal Care. 2007;
- Millichap JJ, Millichap JG. Clinical features and evaluation of febrile seizures. In: UpToDate. 2014.
- Leung AKC, Hon KL, Leung TNH. Febrile seizures: An overview. Drugs in Context. 2018.
- Shearer P, Park D, Bowman A, RN BSN, CEN C, CCRN-CMC BC, et al. Seizures and Status Epilepticus: Diagnosis and Management in the Emergency Department. Emerg. med. pract. 2006.
- Duffner PK, Berman PH, Baumann RJ, Fisher PG, Green JL, Schneider S, et al. Clinical practice guideline - Neurodiagnostic evaluation of the child with a simple febrile seizure. Pediatrics. 2011.
- Abend NS, Loddenkemper T. Management of pediatric status epilepticus. Current Treatment Options in Neurology. 2014.
- Sexton DJ. Lumbar puncture: Technique; indications; contraindications; and complications in adults. UptoDate. 2011.
- Loddenkemper T. Febrile status epilepticus: Time is of the essence. Epilepsy Currents. 2014.
- Offringa M, Newton R, Cozijnsen MA, Nevitt SJ. Prophylactic drug management for febrile seizures in children. Cochrane Database of Systematic Reviews. 2017.
- Rosenbloom E, Finkelstein Y, Adams-Webber T, Kozer E. Do antipyretics prevent the recurrence of febrile seizures in children? A systematic review of randomized controlled trials and meta-analysis. Eur J Paediatr Neurol. 2013;
- Knudsen FU. Febrile seizures treatment and outcome. Brain Dev. 1996;
- Patel N, Ram D, Swiderska N, Mewasingh LD, Newton RW, Offringa M. Febrile seizures. BMJ (Online). 2015.
- Verity CM, Greenwood R, Golding J. Long-term intellectual and behavioral outcomes of children with febrile convulsions. N Engl J Med. 1998;
- Martinos MM, Yoong M, Patil S, Chin RFM, Neville BG, Scott RC, et al. Recognition memory is impaired in children after prolonged febrile seizures. Brain. 2012;
- Fetveit A. Assessment of febrile seizures in children. European Journal of Pediatrics. 2008.
- Camfield P, Camfield C. Febrile seizures and Genetic Epilepsy with Febrile Seizures plus (GEFS+). Epileptic Disord. 2015;
| Table 1: Pediatric Vital Signs Normal Ranges | Heart Rate (beats/min) | Respiratory Rate (breaths/min) | Blood Pressure (mmHg) |
| Neonate | 90-205 | 30-53 | 67-84 / 35-53 |
| 1-12 Months | 90-190 | 30-53 | 72-104 / 37-56 |
| 1-2 Years | 80-140 | 22-37 | 86-106 / 89-112 |
| 3-5 Years | 65-120 | 20-28 | 89-112 / 46-72 |
| 6-11 Years | 58-118 | 18-25 | 97-120 / 57-80 |
| 12-15 Years | 50-100 | 12-20 | 110-131 / 64-83 |

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.