Approach to
Fall in an elderly patient
Melanie Leung1
Published online: 12 June 2021
1Department of Medicine, McGill University, Montreal, Quebec, Canada
Corresponding Author: Melanie Leung, email melanie.leung@mail.mcgill.ca
DOI: 10.26443/mjm.v19i1.313
Abstract
25% of elderly adults fall every year. As most of disease entities seen in Geriatrics, falls are often multifactorial. A systematic approach is therefore key to identify causes and address them. This review summarizes the main causes of falls in the geriatric population, an approach for work-up, and key aspects for its management and prevention.
Tags: Geriatrics, Fall, Elderly
Question
An 80-year-old man who did not seek medical attention for several years presents to the Emergency Department for recurrent falls at his house. His past medical history includes hypertension, dyslipidemia, ischemic stroke (2 years ago), COPD, diabetes, and BPH with a history of urinary retention 6 years ago. He had cataract surgery in his left eye 1 year ago. He weighs 80 kg and measures 1.65 m tall. His medications are:- Perindopril 4 mg + Indapamide 2.5 mg PO daily
- Rosuvastatin 40 mg PO daily
- ECASA 80 mg PO daily
- Inspiolto 2.5 mcg + 2.5 mcg INH daily
- Pantoprazole 40 mg PO daily
- Metformin 850 mg PO BID
- Glyburide 10 mg PO BID
- Tamsulosin 0,8 mg PO daily
- Dutasteride 0,5 mg PO daily
- Lorazepam 1 mg po QHS regular
- Vitamin D 10,000 units qweek
- Acetaminophen 650 mg PO QID regular
- Hb 100 g/L (normal 130-170)
- MCV 115 fL (normal 80-100)
- Platelets: 380x109/L (normal 130-400)
- WBC: 7x109/L (normal 4-10)
- Na 141 mmol/L (normal 136–146 mmol/L)
- K 4.0 mmol/L (normal 3.5–5.1 mmol/L)
- Urea 8.1 mmol/L (normal 2.1–8.0 mmol/L)
- Cr 99 μmol/L (normal 49–93 µmol/L)
- Cl 100 mmol/L (normal 98–107 mmol/L)
- Ca total 2.40 mmol/L (normal 2.12–2.52 mmol/L)
- Mg 0.65 mmol/L (normal 0.74–1.03 mmol/L)
- PO4 1.41 mmol/L (normal 0.81–1.58 mmol/L)
- HCO3 26 mmol/L (normal 21–32 mmol/L)
- Glucose 6.0 mmol/L (normal 4.0–11.0 mmol/L)
- CK 320 IU/L (normal 30–250 IU/L)
- Measure serum vitamin B12 level
- Perform EKG
- Perform CT head without contrast
- Start IV fluids
- All of the above
- All of the above except c
Answer
Based on the clinical presentation, multiple diagnoses can be suspected. The patient has orthostatic hypotension since his systolic BP drops over 20 mm Hg and his heart rate increases over 20 beats per minute when standing from a seated position. It might be caused by polypharmacy including his antihypertensive medication and α-1 blocker, as well as by dehydration, which is reflected in the elevated CK, Cr and urea. Other medications, such as benzodiazepines, can also cause falls. Therefore, medication review and IV fluids can be helpful. A systolic murmur has been identified and warrants further investigation with ECG as the first step. The macrocytic anemia with signs of peripheral neuropathy suggests vitamin B12 deficiency, so serum levels should be measured. In this situation, a CT head is not absolutely indicated, given the absence of focal neurological deficit and normal level of consciousness.
Initial Approach
Falls, like any geriatric syndrome, is often multifactorial. It is often the result of several predisposing factors, which puts the patient at increased risk of falls, and of a precipitating factor, which is commonly an environmental hazard or an acute or worsening medical condition. (1-5) Therefore, evaluation of a patient with falls starts with a complete history and physical examination.
History of previous fall(s) and near-falling
For each fall, the following components should be covered: time (year, month), any medical visits or hospitalizations, activity of the patient at the time of fall, prodromal symptoms (e.g. light-headedness, difficulty breathing), location of the fall (indoors? outdoors? anything on the floor that precipitated the fall?), mechanism of fall (e.g. whole body on the ground? outstretched hands?), loss of consciousness, and change in medication. Loss of consciousness suggests orthostatic hypotension, cardiac and/or neurological disease, and potentially serious injuries from the fall. (1-4)
Environmental hazards
These hazards are defined as any item or situation in the environment that puts one at risk of falls. One can ask about rugs, slippery or uneven floors or bath tub, or difficult stairs. (1-5)
Activities of daily living (ADLs) and instrumental activities of daily living (iADLs)
Asking about ADLs and iADLs are essential when assessing any elderly patient. They portrays the functionality of a patient and reflect his/her social environment. Limitations in ADLs and iADLs points to some impairment (e.g. cognitive, mobility) and helps to guide management, such as the involvement of other health professionals including an occupational therapist, physiotherapist, or social worker. ADLs include bathing, dressing, eating, urinary/fecal continence, and mobility. iADLs include cooking, shopping, managing medications, managing finances, housework, and transportation. (1-4)
Orthostatic hypotension
Orthostatic hypotension should be evaluated for any patient presenting after a fall. It is a quick, easy, and readily available test that can be performed in virtually any setting. It constitutes an important and reversible cause for falls. To evaluate for orthostatic hypotension, the patient should be supine for 5 minutes before blood pressure and heart rate are measured. Then, the patient stands up and vital signs are measured once more within 2 minutes of standing. A patient meets criteria for orthostatic hypotension if the systolic blood pressure drops ≥20 mm Hg, the diastolic blood pressure decreases ≥10 mm Hg, or the heart rate rises ≥20 beats per minute. Once a diagnosis has been established, clinicians should look for its cause, which is commonly autonomic dysfunction, medications, or dehydration. Medications that frequently cause orthostatic hypotension include tricyclic antidepressants, anxiolytics, levodopa, diuretics. Autonomic dysfunction can be screened by asking for symptoms of dizziness, loss of consciousness, incontinence, constipation, and impotence. It can take place in the context of diabetes, vitamin B12 deficiency, stroke, multiple system atrophy, or Parkinson’s disease. (1-6)
Gait, balance, and lower extremity strength
Assessment for these components should start with a thorough history. The clinician should ask questions about difficulty with balance/walking, use of assisting devices, level of mobility (e.g. bed-bound? chair-bound? regular exercise?), and environmental hazards (e.g. carpets). Then, on physical exam, the following components are routinely assessed: a) observation of gait (asymmetry, wide base, slow, shuffling, posture, arm swinging), b) Romberg, c) Timed Up and Go, d) 30-second chair stand, e) 4-stage balance. (1-4)
Vision
Decreased visual acuity, defined as a visual acuity of 20/40 and less, impairs the sensory part of balance and can prevent one from adequately assessing the environment. Visual acuity can be assessed with a Snellen chart. Patients wearing glasses at the time of fall should keep them on during the assessment. Each eye should be evaluated separately. Visual fields should also be assessed. Interestingly, multifocal lenses, or lenses containing multiple prescriptions, are not recommended when walking outdoors and going up/down the stairs as they are found to increase the risk of falls. (1-5)
Audition
Impaired hearing capacity may suggest a deficit in the vestibular system. Hearing can be tested via the whisper test: the examiner stands at arm length behind the patient and while the opposite ear is occluded, the examiner orates some words or numbers that the patient has to repeat. If the test is abnormal, Rinne and Weber tests can be performed to distinguish sensorineural from conductive hearing loss. (1,3,4)
Feet and footwear
Foot deformities (e.g. callouses, arthritic deformities) and inappropriate footwear impair the contact between the feet and the floor. Poorly-fitted footwear, high heels, and unlaced shoes are associated with an increased risk of falls. Additionally, sensory function in the feet should be tested, as proprioception can be impaired in diabetes, vitamin B12 deficiency, and other diseases. (1-5)
Cognition
Dementia can impair environmental awareness and/or create neurological deficits. Cognition can be assessed with Folstein’s Mini Mental State Examination. An abnormal score is ≤25. If a patient scores well but dementia is still suspected, a MOCA can be performed to test executive function. (1-5)
Medication review
Polypharmacy, defined as the daily intake of ≥5 medications, particularly affects elderly individuals. It is important to pay close attention to medications causing sedation, confusion, or orthostatic hypotension, and to medications that interact with alcohol and other medications. To help with medication selection, the American Geriatrics Society developed Beers Criteria. Medications strongly linked with falls include SNRIs, opioids, benzodiazepines, and “Z-drugs” (Eszopiclone, Zaleplon, Zolpidem). Over-the-counter drugs should also be considered (e.g. dimenhydrate, diphendramine).
Patient compliance should also be evaluated. Poor patient compliance can lead to exacerbation of medical illness and precipitate falls. Notably, elders are recommended to take vitamin D supplements, especially in Northern countries where exposure to sunlight is limited. Deficiencies in vitamin D cause neuromuscular dysfunction, decreased muscle strength, and increased risk of osteoporosis. (1-7)
Investigations
There is no consensus on lab tests and imaging modalities that should be performed in the setting of falls. The following are investigations commonly ordered:
- CBC: Hemoglobin can help support the diagnosis of anemia or of hemoconcentration, suggesting dehydration. If anemia is diagnosed, the mean corpuscular volume can be helpful in determining the cause of anemia. For patients presenting after a fall, special consideration should be given to macrocytic anemia associated with vitamin B12 deficiency as it can cause peripheral neuropathy. (2)
- Creatinine kinase (CK): CK is an essential enzyme for muscle contraction. Elevated CK can be seen in rhabdomyolosis, dehydration, and with use of statins. Serum CK level can help to estimate the timing of falls, especially if the patient lost consciousness or was unwitnessed. (8)
- Chem10: Abnormalities in electrolytes can reveal renal injury. Hypoglycemia may precipitate a fall, and hyperglycemia may hint diabetes and the possibility of peripheral neuropathy. (2)
- CT head: This investigation is not routinely performed for elders presenting after a fall. The indications are decreased consciousness, focal neurological deficits, and history of post-traumatic lesion. The use of antiplatelet or anticoagulant is not an absolute indication but should be considered. (9)
- EKG: EKGs can help to identify arrhythmias that might have caused a syncope-associated fall. (1-5)
Beyond the Initial Approach
This section covers special considerations for the management of important causes of falls in the elderly population.
- Orthostatic hypotension: Educate patients to rise slowly from bed or chair and to take a pause prior to walking. Elastic stockings and adequate hydration (i.e. 1.5-2L/day with adjustments based on the patient’s medical conditions) are recommended. The clinician should discharge any non-essential medication or reduce dosage if possible. If hypotension is persistent despite these interventions, patients can be started on midrodrine (an adrenergic α1-agonist) or fludrocortisone (a synthetic mineralocorticoid). (1-6)
- Difficulty with gait or balance: Involve physiotherapists and occupational therapists to help patients with mobility reconditioning and to assess patients’ needs in terms of living environment. (1-4)
- ADLs and iADLs: If a patient requires regular assistance, lives in a setting that is inappropriate for their needs, or is suspected of suffering from abuse or neglect, social workers should be involved. Close family members can also be consulted. (1-4)
- Vision: An eye exam every 1-2 years is recommended. If cataract is suspected, refer to an ophthalmologist. (1-5)
- Audition: If vestibular dysfunction is suspected, refer to an otolaryngologist. (1,3,4)
- Feet and footwear: Counsel patients to not walk barefoot or in stockings as these modalities are more slippery and the risk of infection/injury is higher. Recommend foot care with a podiatrist. (1-5)
- Medication review: A medication review should be done for every patient and if available, pharmacists can be consulted. If discontinuation of a medication is chosen, gradual tapering down might be required to prevent withdrawal. If there are issues with patient compliance, dispills can be helpful and local community centers can also provide assistance with medication administration. (1-6)
- Environmental hazards: Involvement of an occupational therapist is recommended for a complete assessment of environmental hazards. Night lights are suggested. Consider involving social work if the patient’s living situation is not considered appropriate for his/her needs. (1-5)
- Elevated CK: Generous hydration is recommended, whether oral or intravenously. (8)
- Hypoglycemia: Ensure appropriate food intake and adjust diabetic medications if needed. (10)
- Hyperglycemia: Measure HbA1c and adjust medication if needed.
- If abnormal CT head: Consider consultations with Neurology and Neurosurgery. If a bleed is observed (see Figure 1), arrest antiplatelet and anticoagulation therapies. (9)
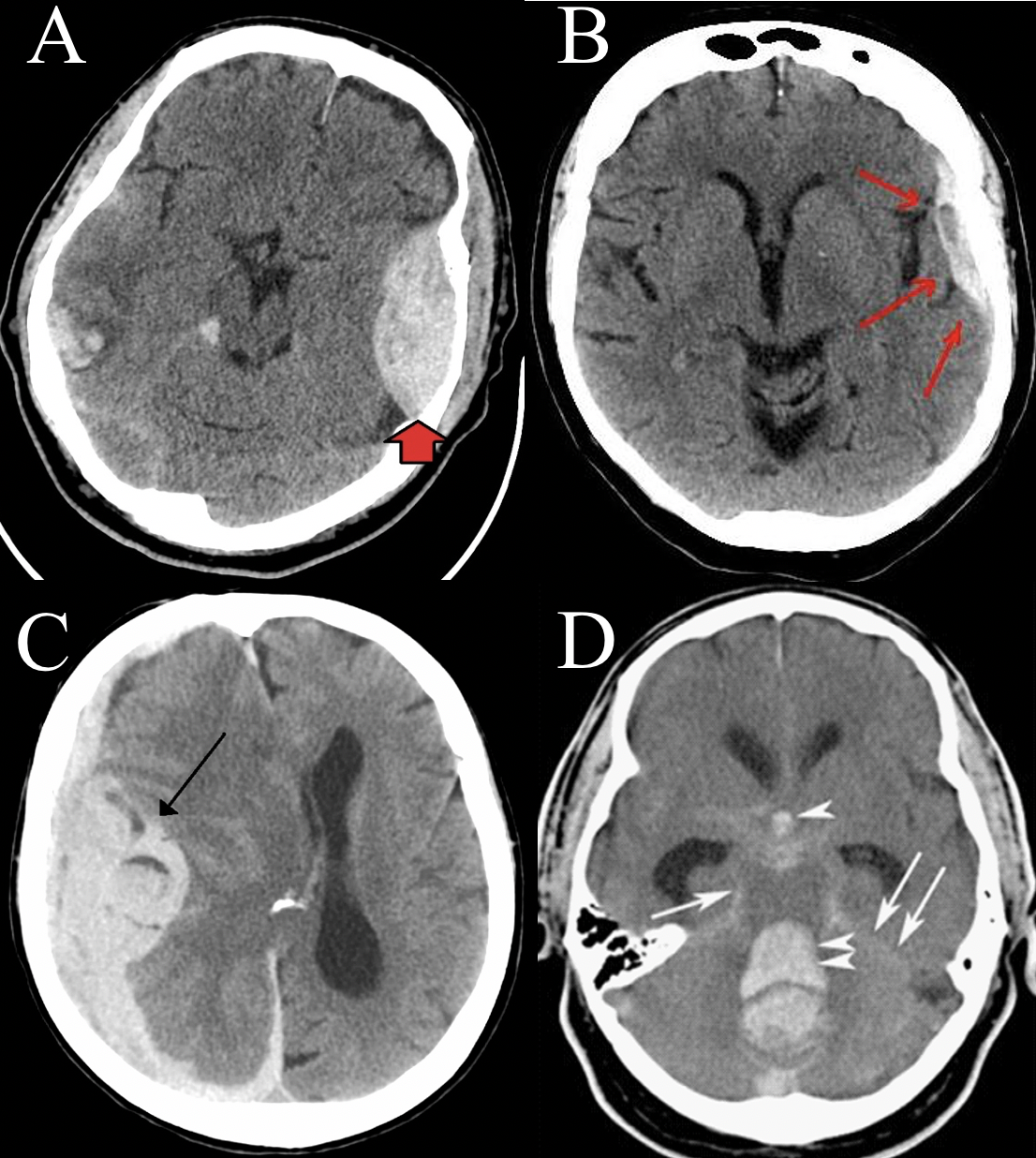
- Epidural hematoma. (11)
- Subdural hematoma. (12)
- Intracranial hematoma. (13)
- Subarachnoid hematoma. (14)
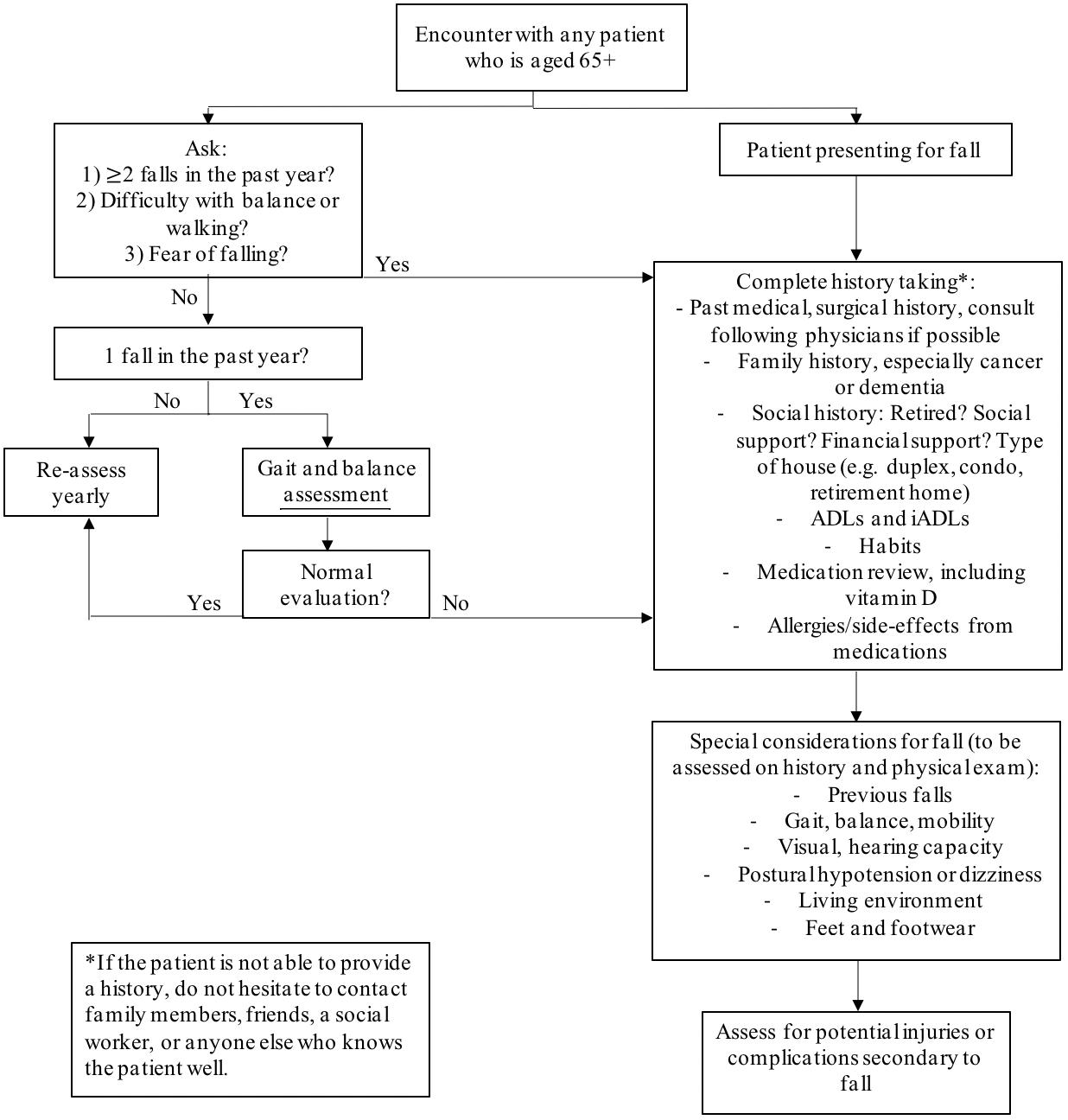
Adapted from: Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. (4)
References
- CDC [Internet]. USA: c2020. Material for Healthcare Providers | STEADI – Older Adult Fall Prevention | CDC Injury Center [cited 2020 September 2]; [about 1 screen]. Available from: https://www.cdc.gov/steadi/materials.html
- Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall?. Jama. 2007 Jan 3;297(1):77-86.
- Ganz DA, Latham NK. Prevention of falls in community-dwelling older adults. New England journal of medicine. 2020 Feb 20;382(8):734-43.
- Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. Journal of the American Geriatrics Society. 2011 Jan;59(1):148-57.
- Tinetti ME. Preventing falls in elderly persons. New England journal of medicine. 2003 Jan 2;348(1):42-9.
- Lipsitz LA. Orthostatic hypotension in the elderly. New England Journal of Medicine. 1989 Oct 5;321(14):952-7.
- 2019 American Geriatrics Society Beers Criteria® Update Expert Panel, Fick DM, Semla TP, Steinman M, Beizer J, Brandt N, Dombrowski R, DuBeau CE, Pezzullo L, Epplin JJ, Flanagan N. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society. 2019 Apr;67(4):674-94.
- Wongrakpanich S, Kallis C, Prasad P, Rangaswami J, Rosenzweig A. The study of rhabdomyolysis in the elderly: an epidemiological study and single center experience. Aging and disease. 2018 Feb;9(1):1.
- Pages PJ, Boncoeur-Martel MP, Dalmay F, Salle H, Caire F, Mounayer C, Rouchaud A. Relevance of emergency head CT scan for fall in the elderly person. Journal of Neuroradiology. 2020 Feb 1;47(1):54-8.
- Meneilly, G. S., Knip, A., Miller, D. B., Sherifali, D., Tessier, D., \& Zahedi, A. Diabetes in older people. Canadian journal of diabetes. 2018; 42: S283-S295.
- Search results for “epidural hematoma”. Commons Wikimedia; 2018 April 4. Available: https://upload.wikimedia.org/wikipedia/commons/f/f9/EpiduralHematoma.jpg (accessed 2020 Sept. 8).
- Search results for “subdural hematoma”. Commons Wikimedia; 2008 July 22. Available: https://upload.wikimedia.org/wikipedia/commons/5/57/Ct-scan_of_the_ brain_with_an_subdural_hematoma.jpg (accessed 2020 Sept. 8).
- Search results for “intracranial hematoma”. Commons Wikimedia; 2011 August 29. Available: https://upload. wikimedia.org/wikipedia/commons/d/d8/Intracranial_bleed_with_ significant_midline_shift.png (accessed 2020 Sept. 8).
- CT_of_subarachnoid_hemorrhage. Commons Wikimedia; 2016 July 25. Available: https://commons.wikimedia.org/wiki/File:CT_of_subarachnoid_hemorrhage.png (accessed 2020 Sept. 8).

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.