Scoping Review
Children’s health-related experiences in India
Yi Wen Wang1
Published online: 25th November 2023
1Shriners Hospitals for Children, Canada
2McGill University, Montreal, Canada
3Department of Medical Oncology, Max Super Speciality Hospital, Saket, New Delhi
Corresponding Author: Yi Wen Wang, email: yi.wen.wang@mail.mcgill.ca
DOI: 10.26443/mjm.v21i1.1004
Abstract
Background & Objectives: The perspectives of children have becoming increasingly emphasized in healthcare research and practice in order to facilitate children’s inclusion, participation, and decision-making in matters related to their health. In India, however, little is known about children’s views regarding their health despite the various health challenges and ethical concerns they may face, such as poverty, malnutrition, and gender inequalities. The aim of this scoping review is to explore children’s health-related experiences from their own perspectives in India from 2000 to 2020.
Methods: Five online databases were searched. Three independent reviewers screened articles for inclusion. Included texts were analyzed using thematic synthesis, which involved extracting and descriptively coding data, categorizing/grouping codes by similar topics, and comparing and contrasting topics to generate descriptive themes. The scoping review was reported using the PRISMA-ScR checklist.
Results: Fifty-two articles were included, and five descriptive themes were identified. The articles typically overlapped in themes, which related to children’s health-related experiences (n=38), emotions (n=19), and knowledge (n=15); the impact of illness on children’s lives (n=41); and children’s ability to communicate their needs (n=12).
Interpretation & Conclusions: We identified the need to tailor research designs to better elicit children’s perspectives and provide comprehensive health education for children and families in India. This scoping review helped to highlight gaps in healthcare policy, practice, and research, providing a starting point for more focused investigation into children’s health-related experiences in India.
Tags: India, Children’s healthcare, Scoping review, Child ethics, Lived experience
Introduction
Childhood ethics is an emerging field of inquiry with a paucity of research examining health-related experiences from the child’s perspective. (1) A child’s perspective is defined as a direct view on “conditions, experiences, perceptions and actions, based on what he or she finds important”. (2) Children’s perspectives are being increasingly utilized to promote their participation, inclusion, and agency within fields such as education, health, and law. (1) According to the World Health Organization, (3) health extends beyond the simple absence of disease and encompasses physical, mental, and social well-being. The concept of whole person well-being involves various domains of one’s life, including physiological and psychological processes, as well as physical, sociocultural, and spiritual environments. (4) Therefore, an individual’s well-being can be deeply affected by their interpretation of day-to-day events, which may align with or go against personal values and beliefs. (5)
Ethics play an integral role in health care and services as healthcare providers must make decisions in patients’ best interests by seeking to reduce harm and maximize benefit. The act of genuinely hearing, acknowledging, and addressing a patient’s voice is therefore critical toward understanding a child’s particular experiences, aspirations, and concerns. This helps to inform an individualized determination of their best interests, which should orient treatment decision-making and is particularly relevant for children who are vulnerable given their development, status as minors and limited legal decision-making capacities within healthcare contexts. (6) However, children with chronic illness have reported being excluded from decisions, discussions, and actions related to their care. This compromises clinicians’ and parents’/caregivers’ abilities to understand children’s perspectives and in turn, their best interests, while leading to feelings of frustration, anger, and fear in children. (7) Nonetheless, young people have clear ideas regarding how their treatment can be improved (8) and have expressed desires for their voices to be heard in healthcare settings. (9) Given that self-management capacities and self-efficacy are positively correlated with health-related quality of life for children with chronic illness, (10) eliciting children’s perspectives during care may support a sense of control over their health, improve their care, and enhance their quality of life. For these reasons, seeking to understand and render children’s perspectives visible in health-related literature is an important step towards advancing the field of childhood ethics. Despite increasing recognition of the children’s voices in healthcare research and practice, research related to this topic has been geographically limited. In turn, children’s perspectives regarding their health are still unclear in many low- and middle-income countries such as India. India has the largest child population (0 to 18 years) in the world but is also disproportionately affected by poverty, malnutrition, poor access to healthcare, gender inequalities, and other health and ethical concerns. (11–13)
This study presents a scoping review of health-related literature from the child’s perspective in India. This review was conducted by VOICE (Views on Interdisciplinary Childhood Ethics), a group of researchers and community partners committed to advancing the field of childhood ethics and global child health. The goals of this scoping review are to: a) improve our understanding of children’s health-related experiences by exploring the perspectives of children in India with illness, disability, and/or physical symptoms within empirical studies; and b) identify areas for further empirical research and examination of ethical concerns.
Methods
Study design
We conducted a scoping review, also known as a knowledge synthesis design, allowing us to summarize a range of evidence and identify the key concepts underpinning a complex, new, or unfamiliar research topic. (14) The approach of a scoping review is broad and uses purposive sampling to identify evidence and gaps in the literature without a quality appraisal step. (15) The six steps of the scoping review framework are: (a) identifying the research question; (b) identifying relevant studies; (c) study selection; (d) charting the data; (e) collating, summarizing, and reporting the results; and (f) consultation. (14) Our results were reported using the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR; 16) checklist which can be found as a Supplemental Material (File S1).
Identifying the research question
The objective of this scoping review was to explore the existing knowledge about children’s health-related experiences from their own perspectives in India. We aimed to answer the research question: What do we know about children’s health-related experiences in India?
Identifying relevant studies and study selection
For this review, the term ‘children’ referred to individuals between 3 and 17 years of age. Seventeen years was selected as the upper limit for the age range as the age of majority in India is 18 years (i.e., when an individual ceases being a minor). (17) Only empirical studies examining children’s health-related experiences from their own perspective were included (e.g., outlining findings in the child’s own words). No language restrictions were implemented, but the studies were limited to those entirely conducted or at least partly conducted in India and by publication date from 2000 to June 2020. This time period was selected because the interdisciplinary interest in childhood studies emerged recently around the year 2000 (1), yielding an increase in literature exploring children’s voices, agency, and perspectives. Thus, the current literature was seen as providing a synopsis of the state of knowledge on the topic.
Studies that were excluded were opinion papers or studies that were normative in focus (i.e., recognized norms defined by legal, ethical and/or professional practice standards). Moreover, data from infants (0-12 months), toddlers (12-36 months), and children giving opinions on health topics, illnesses, or conditions for which they were not afflicted with were excluded. However, studies with some participants over 18 years of age but which fulfilled the rest of the inclusion criteria were included if most participants in the respective study were under 18 years of age, as these articles still contained valuable knowledge regarding children’s perspectives.
Search strategy
The search strategy paralleled the three-step process outlined by Peters et al. (18) whereby (a) an initial search was run in CINAHL and MEDLINE, (b) a second, comprehensive search was run using keywords derived from the initial search, consultation with a research librarian, and a target article. Then five online databases were searched: CINAHL (1937-2020), Global Health (1973-2020), MEDLINE (1949-2020), PsycINFO (1597-2020), and Web of Science (1900-2020); and (c) reference and citation searching was used to supplement the results from the reference lists in the included studies. (18) Keywords such as “child*”, “India”, “perception*”, and “experience*” were searched within titles and abstracts, reducing the number of irrelevant retrieved articles. The detailed search strategy for MEDLINE can be found in File S2. Endnote X7 software was used to store, organize, and retrieve the search results. Additionally, interlibrary loans were used to locate articles not retrievable in the university collection. Following article retrieval, three independent reviewers screened titles, abstracts, and full-text articles to determine study inclusion.
Charting the data then collating, summarizing, and reporting results
Selected articles were read in full and summarized in a data extraction sheet outlining the: year; study setting; study design and methodology (research type, sample size, data collection methods and tools); population demographics (age range, illnesses/symptoms, healthcare context); qualitative and/or quantitative findings and outcome measures related to children’s perspectives, reports, or understandings of their health-related experiences; and any additional comments or discussion points (e.g., key takeaways, article discussion summary, recommendations and research implications, reviewer questions). The data extraction sheet was created by the first authors (YWW and JB) and tested by charting data from sample articles. The sheet was then reviewed by co-authors and refined in collaboration with the research team to ensure that the contents permitted standardized charting and aligned with our research question. Three authors (YWW, JW, SJ) charted the data. They met regularly with our research team to share their data extraction sheets; discuss and address questions, uncertainties, and concerns; and ensure the charting process remained consistent between the three authors.
The framework for collating and summarizing the results was based on recommendations for enhancing the consistency of scoping review methodologies (19), which includes conducting a descriptive numerical analysis and qualitative thematic analysis guided by our review question. Data analysis was led by the first authors (YWW and JB) in close collaboration with the research team who permitted for member checking and debriefing (i.e., obtaining feedback on data interpretations and analysis); provided input during quantitative and qualitative analysis; and vetted, gave feedback, and provided consensus on generated themes and findings. The descriptive numerical analysis for this scoping review consisted of numerically summarizing the characteristics of the included studies, such as the number of included studies, population demographics, and study designs. (14,19)
A thematic synthesis was conducted whereby the research question guided categorization of the codes and generation of descriptive themes. (20) Data analysis was iterative, inductive, continuous, (1) and conducted in three phases. The first phase included initial open coding, in which data relevant to the review question were extracted from the data extraction sheet and descriptively coded, generating units of analysis or codes. (21) In the second phase, we looked for similarities and differences between codes and grouped similar codes together to form topics, which captured the meaning of the initial code groups. Examples of topics include “impacts of illness on children’s lives”, “children’s physical sensations and symptoms”, and “children’s understanding of their health and illness”. The third phase included relating topics to each other (axial coding), organizing individual topics into themes (thematic analysis), and drawing connections between themes (comparative analysis). (22) This allowed us to generate an understanding of children’s health-related experiences in India and identify areas for further empirical research and ethical examination.
Results
Sample and Study Characteristics
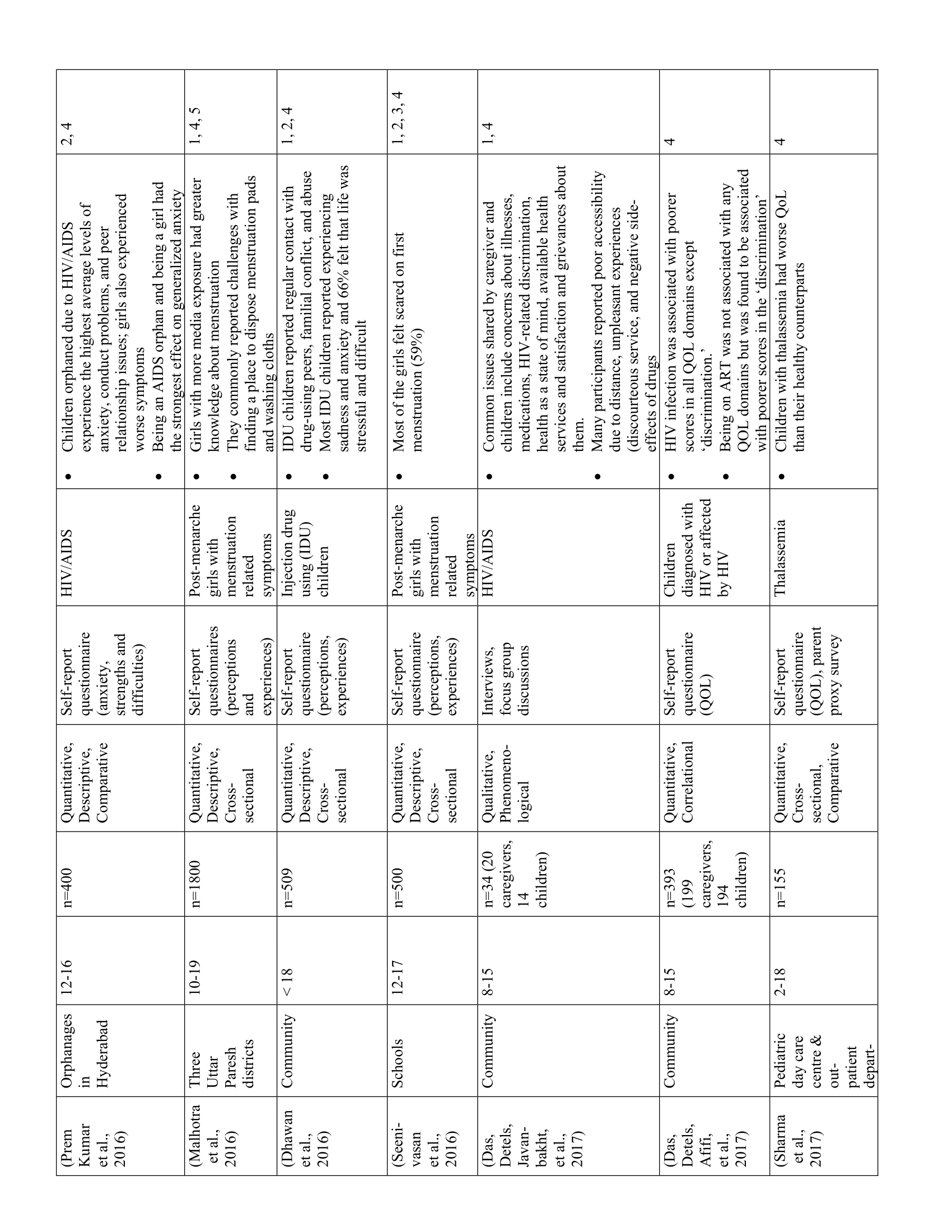
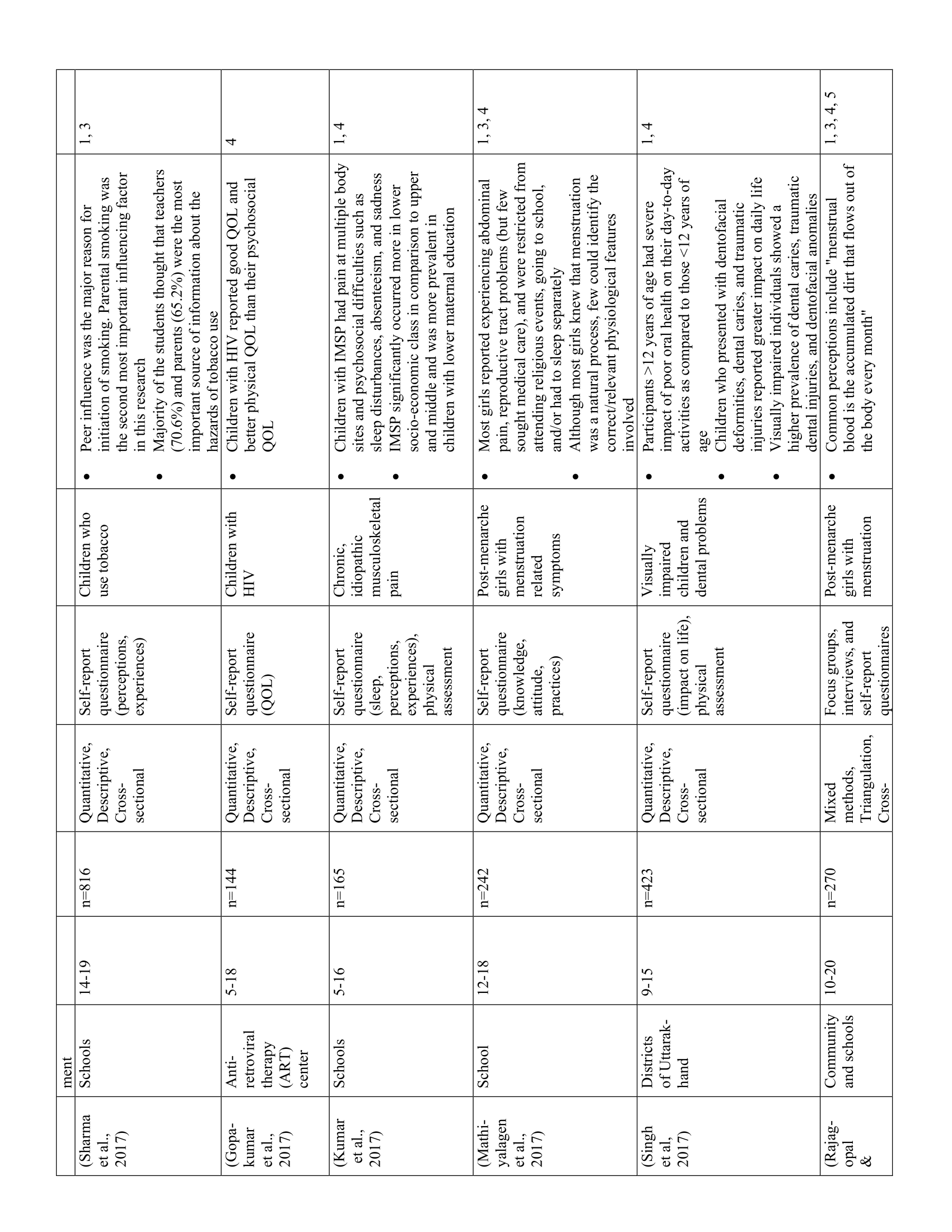
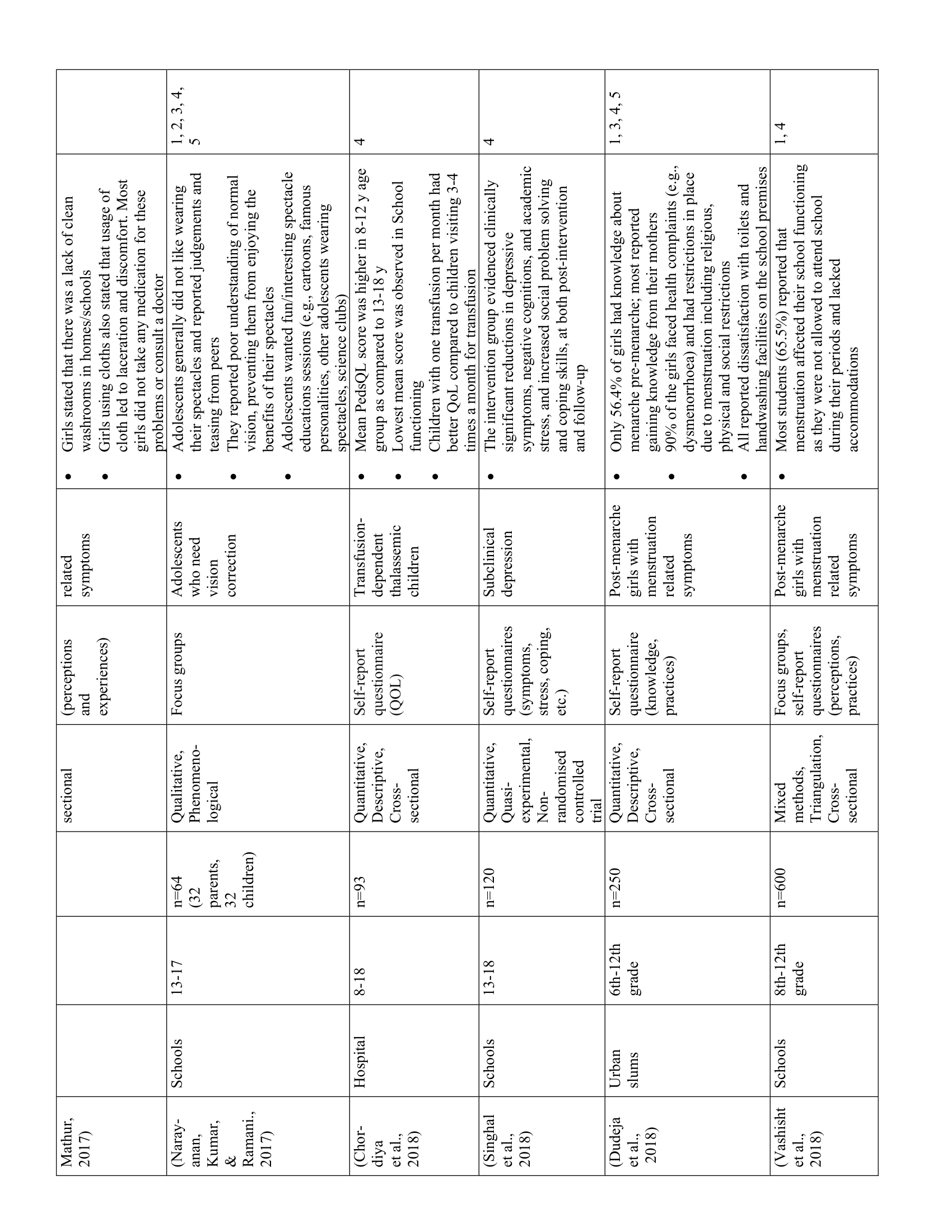
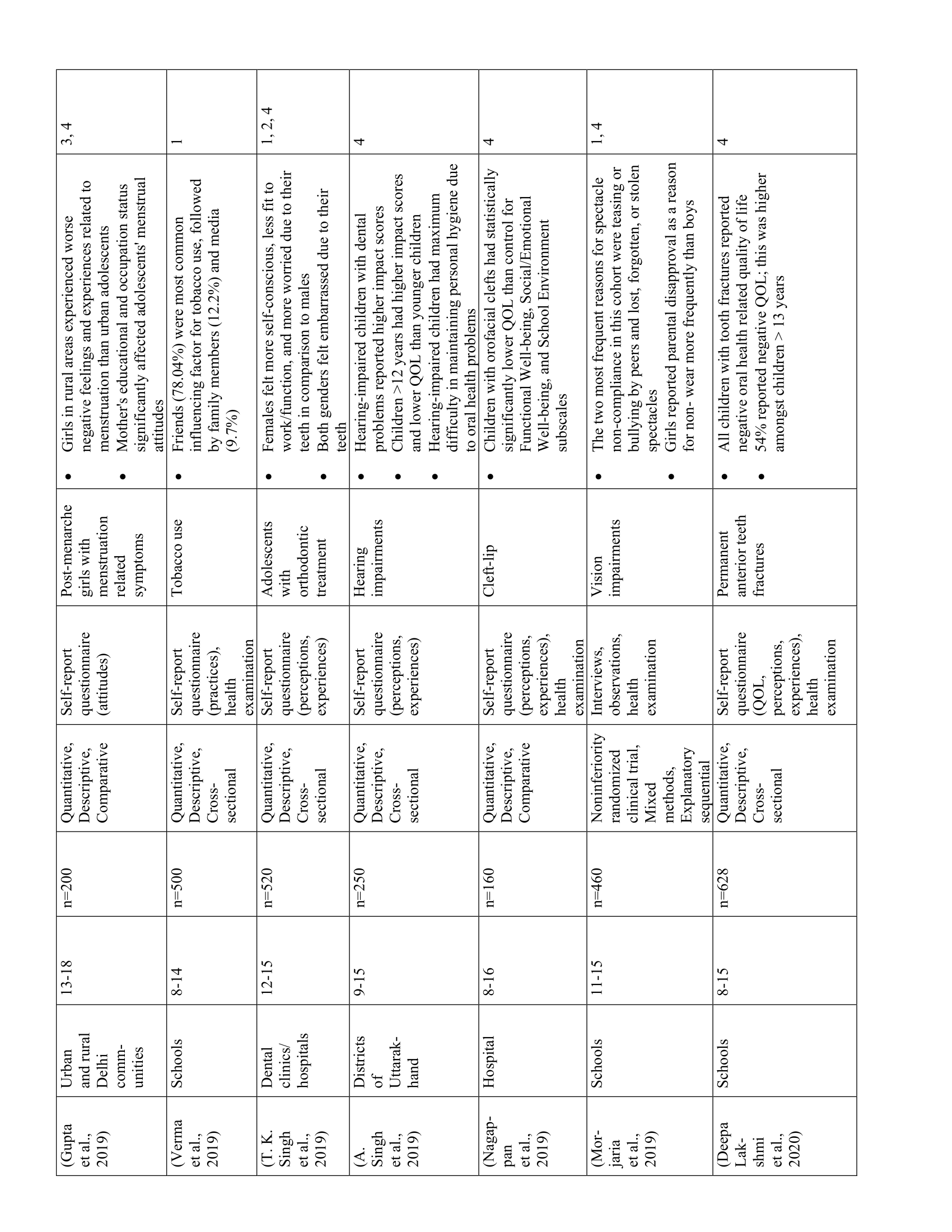
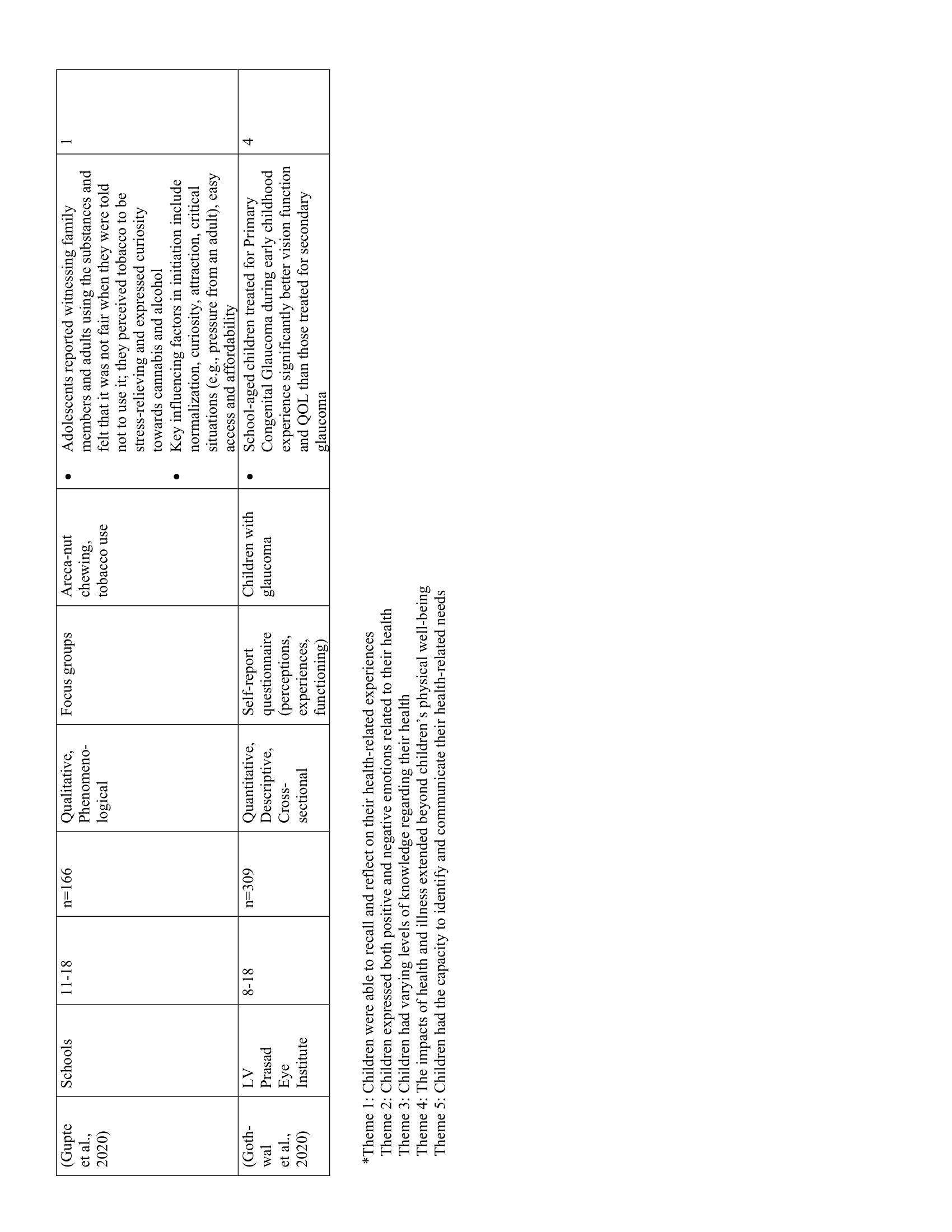
The initial search yielded 11,304 articles. Once duplicates were removed, 10,547 articles were screened based on the inclusion criteria, after which 134 articles remained and were read and assessed in full for eligibility. Finally, 52 studies were included for analysis and summarized in a PRISMA flow diagram (Figure 1). This review synthesized the perspectives of 15,996 children between 3 and 21 years old (inclusive), and was comprised of 37 quantitative studies, 9 qualitative studies, and 6 mixed-methods studies, which were conducted in schools, communities, hospitals, rehabilitation centers, and clinics in both rural and urban settings. Seven studies included some participants above the age of majority (18 to 21 years). Participants had various illnesses and symptoms including asthma, cancer, renal disease, thalassemia, visual impairments, dental issues, leprosy, HIV/AIDS, menstrual symptoms, somatic symptoms, substance-use, depression, musculoskeletal pain, cleft-lip, pregnancy, and mobility impairments/disability.
Thematic Analysis
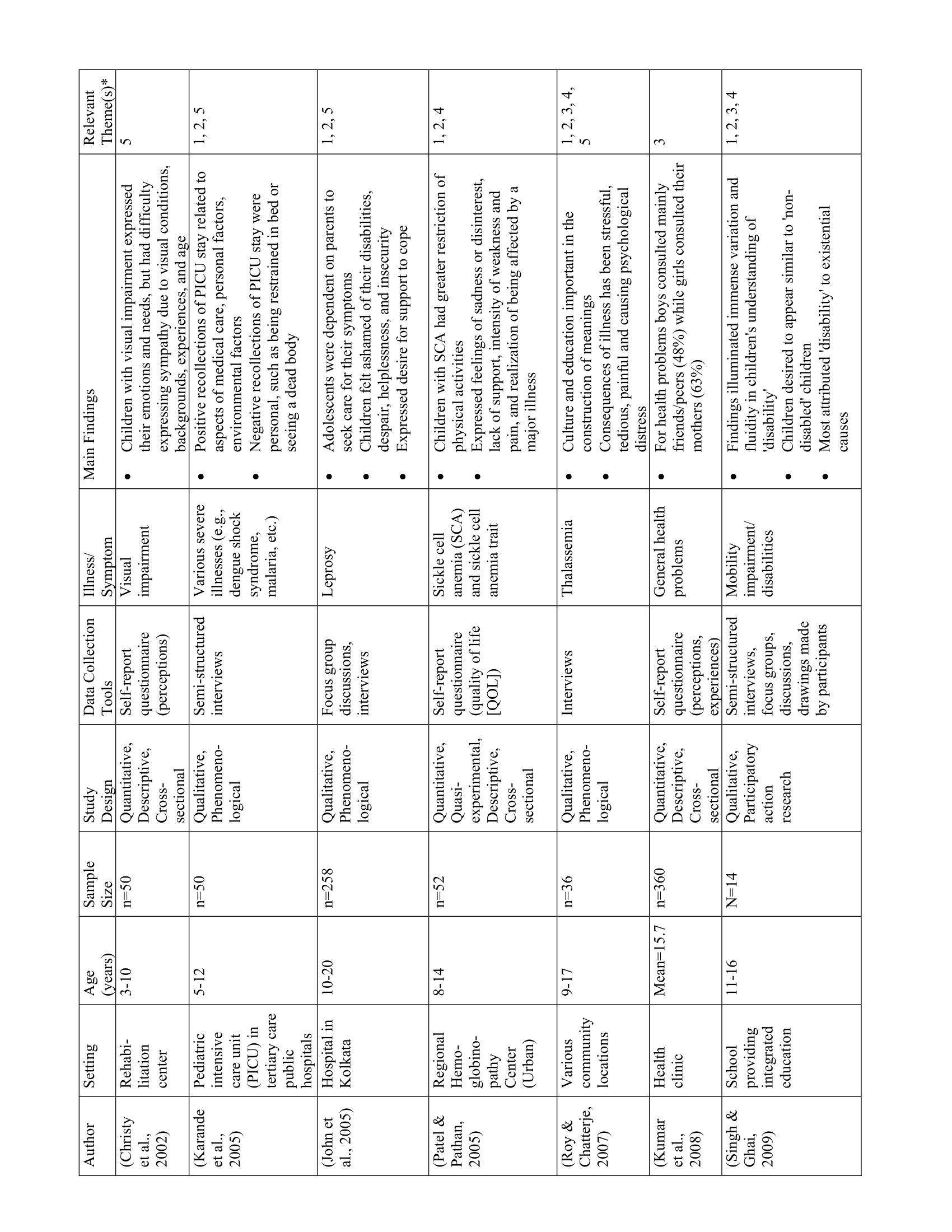
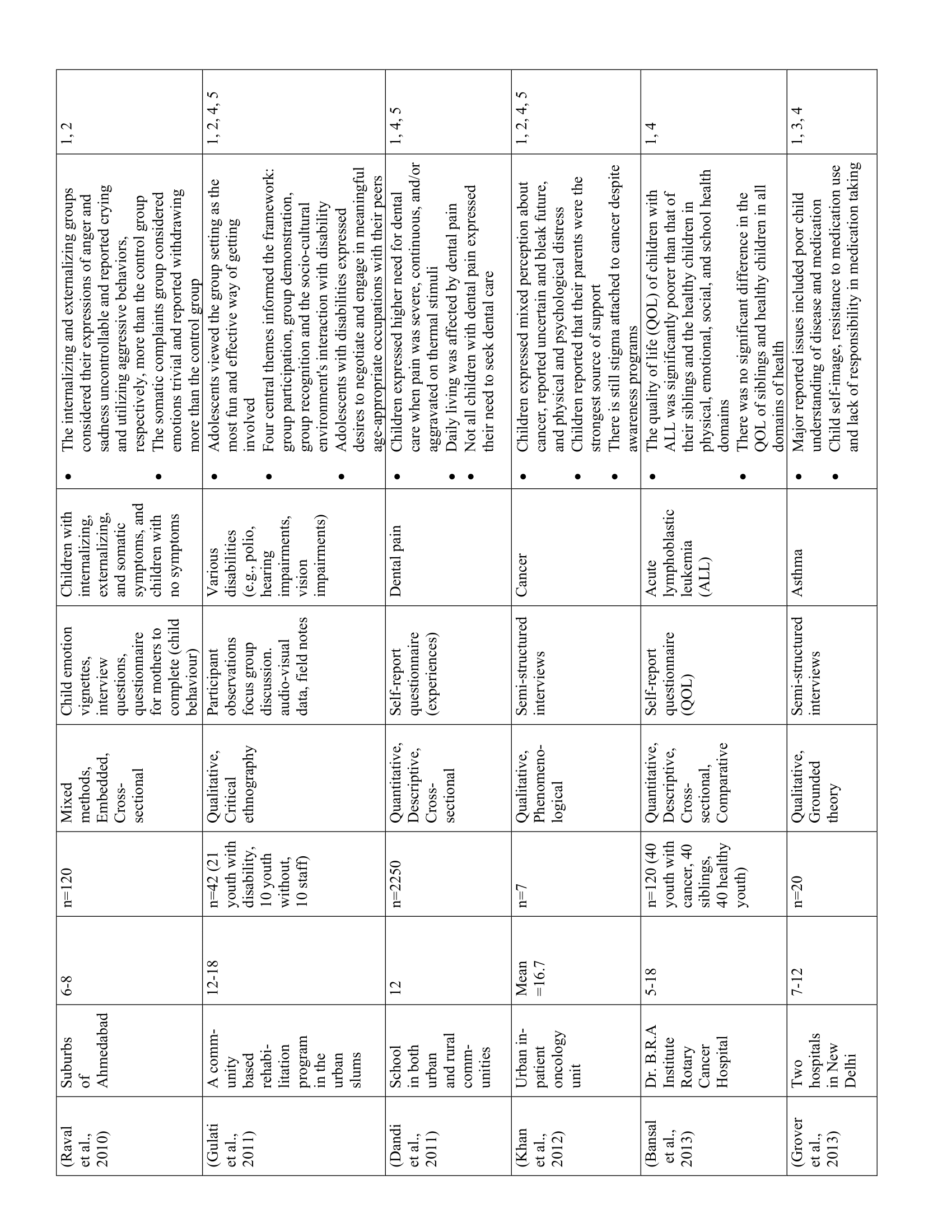
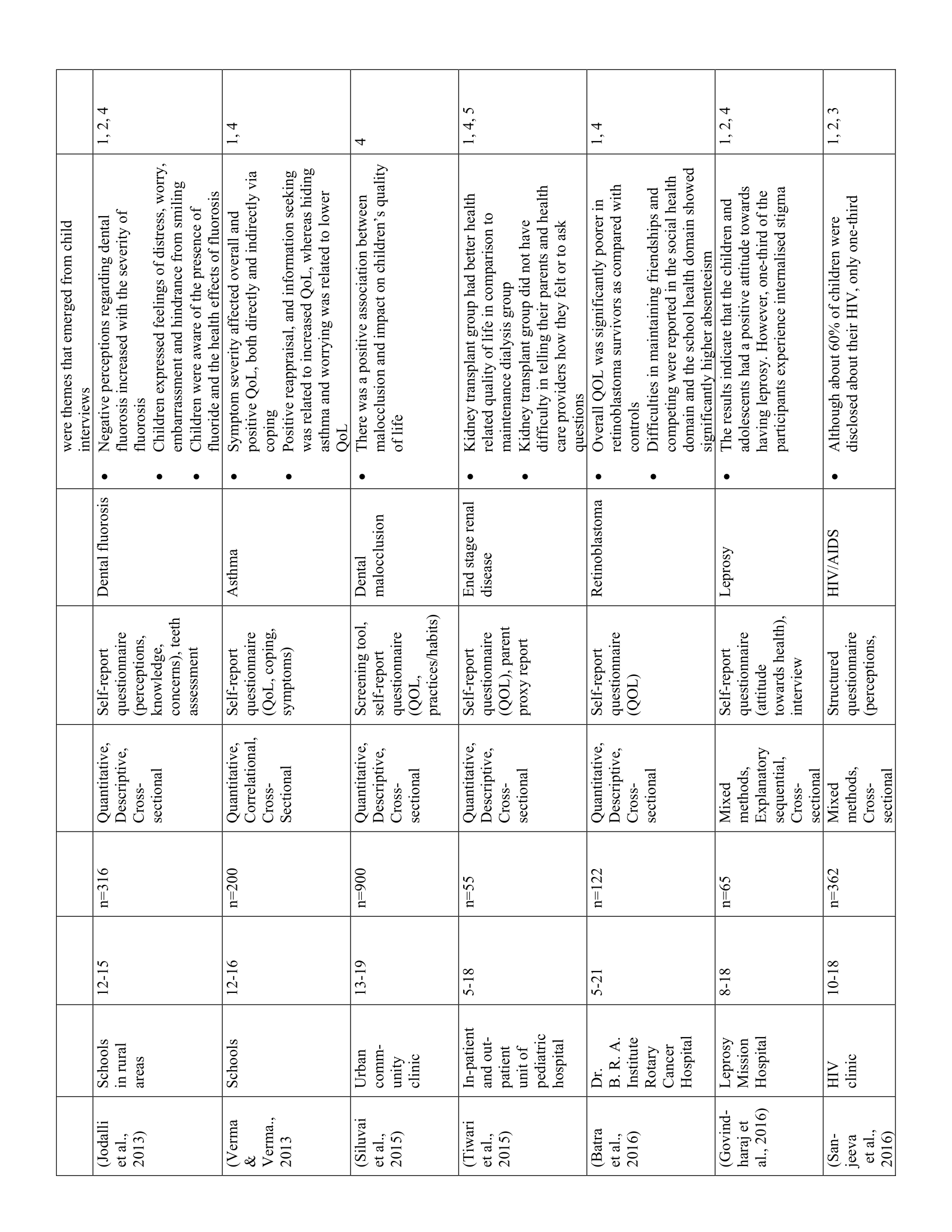
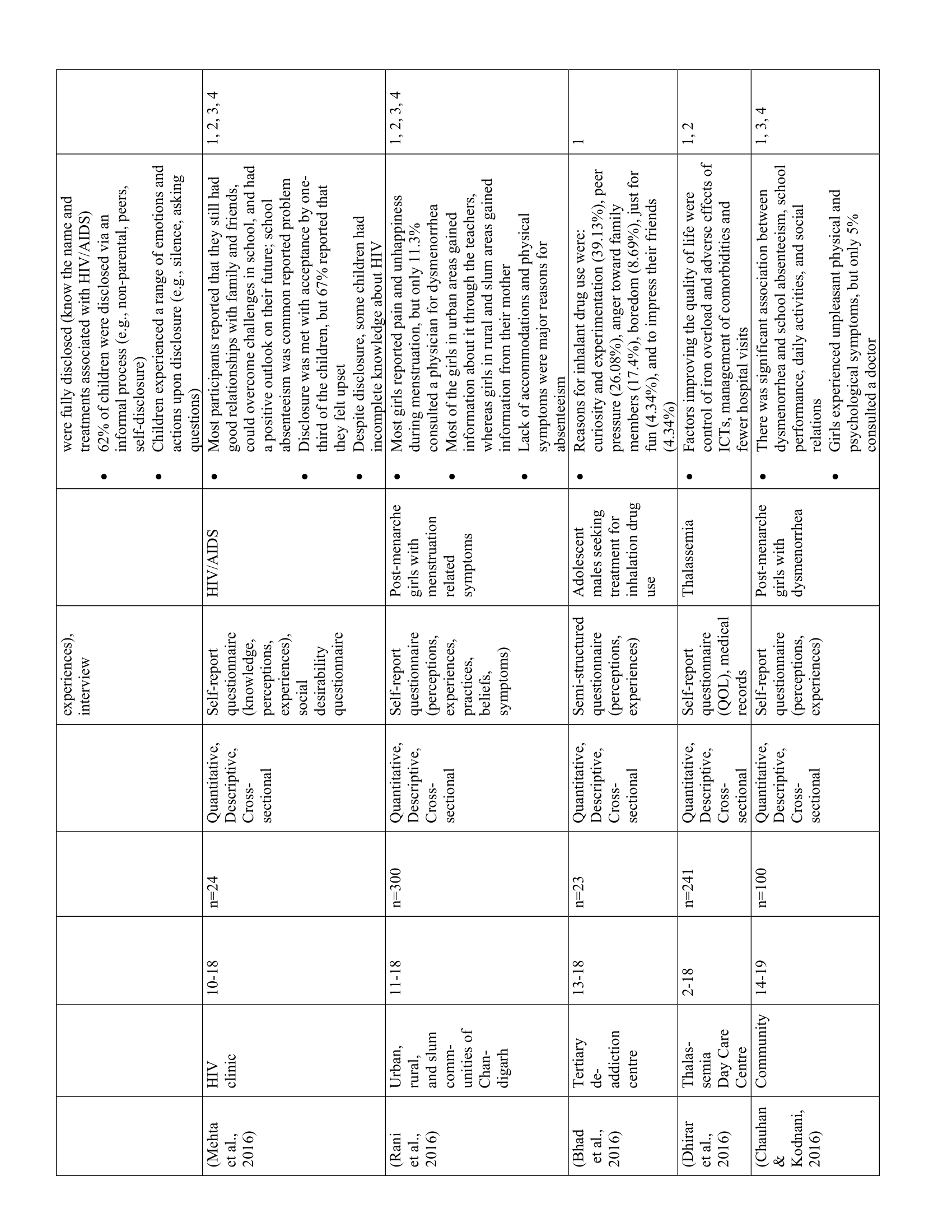
The 52 studies in this review are summarized in Table 1. Five main themes were identified along with 11 subthemes from the extracted codes (Table 2). Each theme was salient to the understanding of children’s health-related experiences and are presented below.
Children recalled detailed health-related experiences in healthcare facilities and communities
Thirty-eight studies showcased children’s abilities to recall and reflect on their health-related experiences. A key similarity between studies was that children were able to describe detailed memories of favourable and unfavourable events related to their medical care, interactions with healthcare staff, and within healthcare facilities. For example, youth living with HIV recounted how discourteous service from healthcare staff left negative impressions of the clinic (23) while adolescents with cancer talked about the debilitating effects of treatment (e.g., oral ulcers, nausea, pain). (24) Conversely, children in PICU recounted comforting actions of nurses and doctors such as speaking nicely and painless injections. (25) Children’s recollections also extended beyond themselves as they described witnessing the experiences of other ill children in the PICU undergoing invasive procedures, injections, and even death. (25)
Within the community, however, children mostly recounted negative experiences related to health barriers and social exclusion. Post-menarche girls, for example, reported having limited access to hygienic facilities at school (e.g., soap, clean water, toilets), prompting them to miss classes during menstruation. (26–29) Children living with HIV/AIDS reported experiencing discriminatory actions from family members including refusals to share food, avoidance, and propagation of misgivings. (23) Finally, children also reported experiencing bullying, teasing, and/or negative judgement from peers due to their symptoms and illness, contributing to absenteeism and treatment non-compliance. (29,30)
Children expressed both positive and negative emotions related to their health
Nineteen studies highlighted children’s expression of positive and negative emotions related to their health. Using interviews, questionnaires, and focus groups, researchers showed that children experienced emotions such as fear, hope, anxiety, hopelessness, insecurity, appreciation, guilt, and sadness towards their health. In general, children’s negative emotions—particularly fear and anxiety—stemmed from unpleasant physical symptoms (e.g., pain, discomfort, nausea), uncertainty about their health and future, and limitations due to dependence on caregivers, activity restrictions, and socioeconomic status. (31–33) Despite the psychological impacts of illness, pediatric PICU patients (25) and children with HIV/AIDS, (34) leprosy, (35) and asthma (36) also reported positive feelings, such as hope and contentment. Examples of when primarily positive emotions arose were when children had a positive outlook on life, (34,36) were knowledgeable about their illness, (35) and felt supported by healthcare providers. (25) While children’s emotions varied with the severity and nature of their illness, their interpersonal experiences, access to resources in healthcare facilities, and communities also contributed to their positive and negative emotions. For example, social exclusion and discrimination led to negative emotions, (29,30) while support and comfort from healthcare providers and family helped to attenuate the negative effects of illness (25, 34-36).
Children had varying levels of knowledge regarding their health, treatment, and the consequences of illness
Fifteen studies showed that children had varying levels of knowledge regarding their health. Children’s beliefs and understanding of their illness and symptoms were shaped by their sociocultural backgrounds. Differences in health-related knowledge were particularly evident in children with thalassemia (37) and post-menarche girls. (32) For example, educated Hindu youth with thalassemia attributed their illness to medical causes, such as lack of prenatal screening. (37) Conversely, Muslim respondents (regardless of education level) believed that their illness was caused by a “sinful past”. (37) For post-menarche girls, perceptions of menstruation varied by maternal education, such that adolescents from rural areas, where women’s educational attainment was typically low, had significantly worse attitudes towards menstruation than their urban counterparts. (32) In particular, rural adolescents were less inclined to ask questions about and discuss menstruation, contributing to a poor understanding of menstrual symptoms, inability to identify organs involved in menstruation, and negative emotions such as feeling “ugly” or “gross”. (32) Regarding other illnesses, such as those with HIV/AIDS or sickle cell hemoglobinopathy, most youth had some knowledge related to medication, treatment, and/or prevention. (34,38,39)
Overall, family, teachers, and friends played the greatest role in children’s health-related knowledge and attitudes. Post-menarche girls, for example, often learned about menstruation from their mothers, (26–28,40). Youth who used tobacco, areca nut (a type of nut with similar properties as nicotine which is usually chewed and can be harmful to one’s health), and other drugs were influenced by friends and/or by witnessing family members use substances. (41–43) These different sources of knowledge influenced the accuracy and scope of children’s health knowledge, as well as their understanding of the importance of treatment and consequences of untreated illness. Although most children understood the severity and impact of their various illnesses, most had incomplete knowledge regarding their symptoms and treatment, which negatively affected treatment seeking, medication compliance, and quality of life. For example, children with asthma commonly reported poor understanding of their disease, contributing to medication resistance. (44) Similarly, children with poor spectacle compliance reported that their parents did not understand their vision problems and that they themselves did not know what “normal” vision was (30) Although post-menarche girls commonly reported experiencing abnormal menstrual symptoms such as UTIs, infections, and lacerations, the vast majority did not seek medical treatment. (45,46)
The impacts of health and illness extended beyond children’s physical well-being
Forty-one studies showcased how the impacts of health and illness extended beyond children’s physical well-being. Children’s various health statuses impacted their physical, emotional, and developmental well-being regardless of illness type and severity. Moreover, children’s well-being varied with age, gender, and socioeconomic status (SES) such that girls, youth 12 years and older, and children with low SES tended to report greater physical and emotional burden and lower quality of life. (32,33,47,48) Although all children reported negative physical sensations such as discomfort, pain, or weakness, they tended to speak more about the impacts of health on their daily activities. Thus, children with health problems (e.g., vision deficits, dental issues, thalassemia, HIV/AIDS) generally reported lower quality of life than their healthy counterparts. (23,42,48,49)
One of the most common issues reported by children was the negative effect of illness on their schooling and relationships with peers. This was particularly salient for children with dental problems, (47) vision impairments, (30) thalassemia, (37) sickle cell hemoglobinopathy, (38) HIV/AIDS, (34) musculoskeletal pain, (50) and unpleasant menstrual symptoms. (29) Children often complained of school absences due to physical symptoms, lack of support, and inadequate facilities to accommodate their health needs. (29,34,50,51) For example, children with sickle cell hemoglobinopathy and thalassemia expressed a lack of support from teachers. (37,38) Children with spectacles reported being teased by school peers (30) and post-menarchal adolescent girls reported having to cope with unhygienic, poorly equipped bathroom facilities that lacked privacy. (29)
Children’s health also impacted their self-perceptions, such that youth with thalassemia, (37) cancer, (24) and sickle cell hemoglobinopathy (38) perceived their diagnosis as a psychological and economic burden for their family and society. Negative self-perceptions usually arose due to feelings of dependence, (24,37) disablement, and guilt. (38) Children’s concerns also revolved around their self-image and desires to be like their “healthy” peers. (44,52–54) While some children with dental fluorosis reported that they liked the appearance of their teeth, others were worried about their appearance. (52) For children with vision impairments, appearance was an important contributing factor towards spectacle non-compliance, particularly amongst girls. (30,55)
Children had the capacity to identify and communicate their health-related needs
Twelve studies highlighted children’s capacity to identify and communicate their health-related needs. Despite the physical and psychosocial challenges associated with ill-health, children were able to identify and communicate their health-related needs when their voices were elicited during interviews, focus groups, or self-report questionnaires. For example, adolescents with thalassemia, (37) cancer, (24) and leprosy (53) demonstrated understanding of their coping needs by expressing their desires for better access to counselling and psychological support. Children’s desires also extended beyond their personal needs: when asked what can be done to improve the intensive care unit, PICU patients suggested implementing “more beds so that more sick children can be in intensive care”. (25)
Although few studies examined children’s communication with healthcare providers, Tiwari et al. (56) found that children with end-stage renal disease were able to ask questions and talk to doctors, nurses, and other staff about their health. Children also revealed the most insight towards their health in group settings with other youth having similar health conditions. For example, results from a focus group study by Narayanan et al. (30) showed that youth with vision deficits had several ideas to encourage spectacle-compliance such as implementing science clubs to deliver education, emphasizing teachers’ roles in the education and encouragement of spectacle-use, and providing trendy frames. Similarly, adolescents with various disabilities (e.g. hearing and vision impairments, and poliovirus) who participated in a community-based rehabilitation programme with other youth, with and without disabilities, provided several insights toward their experiences, desires, and needs. (57) The adolescents reported wanting more education, freedom to engage in day-to-day activities (e.g. social interactions, play, and going outside), and having someone to talk to about their emotions. (57) Despite their restrictions, the youth with disabilities viewed the group setting as a fun and effective way to engage with their community, assume control over their rehabilitation, and take charge of their lives. (57)
Discussion
The purpose of this scoping review was to examine children’s health-related experiences in India, including children’s participation, perceptions, knowledge, and decision-making capacities in matters concerning their health, as well as to identify gaps in the current literature. Despite children’s various health statuses and India’s pluralistic society, (58) children often reported similar health-related experiences, some of which paralleled circumstances in Western societies. (7-10) Overall, the studies were diverse in scope, topic, and focus, consisting of various methodologies and study tools such as self-report questionnaires, focus groups, interviews, participant observations, and children’s drawings. In turn, this scoping review revealed a range of topics related to children’s perspectives such as their recollections, feelings and emotions, and knowledge about their illnesses/symptoms. These aspects shed light on children’s unique perspectives of their health in India, which can serve to enrich our understanding of their best interests. Rendering children’s perspectives visible can influence how healthcare providers and other adults understand and address children’s best interests in the provision of care, which is rooted in childhood ethics.
Most children had clear recollections of their health experiences regardless of illness, symptoms, and surroundings (school, hospital, community). Children and youth were particularly attuned to healthcare providers’ actions, contributing to positive and negative attitudes towards health. For example, children recounted receiving discourteous service from healthcare staff, (23) but also being treated nicely by PICU nurses and doctors. (25) Researchers examining nurse-patient interactions with hospitalized children in Spain reported similar findings, such that children evaluated their treatment based on their perceptions of nurses’ affect, interest, and sympathy towards them. (59) Youth used nurses’ behavioural signals to distinguish between their preferred healthcare providers, contributing towards their treatment compliance and adaptation to hospitalization. (59) Additionally, Ullán et al. (60) found that unlike adults, children appeared to be more sensitive to the “symbolic” aspects of hospitalization, such as the emotional processes, needs, preferences, and behaviours of hospital users. Similarly, the studies in this scoping review highlighted that: a) children were observant of healthcare staff’s behaviours towards themselves and others; and b) their observations directly impacted their emotions and perceptions regarding their health-related experiences.
In the Indian context, parents and peers influenced children’s health-related attitudes, knowledge, and practices. Common challenges including medical non-compliance, poor psychosocial well-being, and lack of health knowledge were often exacerbated by low SES and inadequate support from family, teachers, and friends. These findings align with recent research by Olsen et al., (61) who found that European adolescents who had undergone ulcerative colitis surgery reported feeling “deserted, misunderstood, and ignored” by family and friends due to personal physical changes and school absences. In addition, researchers from Canada and the United States explained that children with a low SES are less likely to have access to medical care, nutrition, and environmental stimuli, increasing the likelihood of injury, mental and physical illness, and developmental delay. (62– 64) Despite some similarities, there were notable differences between children’s health experiences in India and Western countries, particularly related to menstruation and areca nut chewing. For example, American girls/females appeared to be more knowledgeable and accepting of menstruation, (65,66) had greater access to menstrual products (e.g., pads, tampons), (67) and adhered to less strict social restrictions (e.g., being able to attend school and family/religious events) (67) compared to girls from low and middle-income countries. In addition, research on areca nut chewing was limited to South Asia likely due to where it is grown, with only one study conducted in Europe that showed that children who used areca nut were exclusively South Asian. (68)
Finally, although only 16 out of 52 studies elicited children’s health-related opinions via interviews or focus groups, the qualitative and mixed-methods studies showed that children recognized their needs and desires, were insightful when suggesting healthcare changes, and appeared to be more engaged in health discussions in groups settings with other youth. Similarly, Livesley and Long (69) found that hospitalized children in England actively resisted passive roles in healthcare settings and worked hard to assert their competence, knowledge, and capabilities. The notion that peer groups are effective in promoting well-being, knowledge-acquisition and exchange, and collaboration is well supported in research. (70,71) In an overview of loneliness across the lifespan, Qualter et al. (72) described how children increasingly value peer acceptance, intimacy, and social standing as they age. Consequently, disruptions in social functioning by poor health can contribute to feelings of rejection, negative attitudes towards health, and low self-esteem, which were all common issues in this scoping review. The utilization of focus groups to elicit children’s voices therefore supported young people’s psychosocial well-being by providing an safe environment to communicate health concerns and interact with peers. (72–74)
Gaps and limitations
Although we have identified research examining children’s health-related experiences from their perspectives in India, we limited the evidence to empirical studies. Thus, further research into normative standards is required to examine the how notions of participation, inclusion, agency, consent, and assent are viewed in the Indian context, what practices are recommended based upon these views, and if the evidence summarized in this review reflects the adoption of practices. Next, studies were excluded from the review if they examined the health-related knowledge, attitudes, and beliefs of children who were not symptomatic or diagnosed with an illness (e.g., perception of boys towards menstruation). Given the importance of peer relations towards children’s health-related experiences, we recommend an extensive examination of the public health literature. This would provide a more comprehensive understanding of how children perceive their health in India. In terms of methodology, 36 out of 52 studies included in this review used only quantitative methods (e.g., questionnaires, objective medical examinations) to explore children’s health-related experiences, mostly related to quality of life. Although questionnaires are a quick, economic, and effective way to determine individuals’ perceptions regarding a specific topic, questionnaire-use may also lead to bias or reflect the preconceptions of the researcher instead, thus failing to truly capture the participants views, experiences, and voice. (75) Finally, the studies featured in this scoping review were heterogeneous in terms of participant sociodemographic background, illnesses, methodologies, and findings, which precluded our ability to showcase potential relationships between children’s sociodemographic characteristics and contexts (e.g., religion, socioeconomic background, gender/sex) and their health experiences. However, delving into these potential relationships through further empirical studies may help researchers and healthcare providers better understand the unique healthcare needs of children in India.
Future directions and implications for practice
Through this scoping review, we have identified a need for more qualitative, interview-based, and child-centric methodologies (e.g., art, play) in conducting research with children. This will help to fully capture their health-related experiences, promote their inclusion in care, and support the provision of ethical care by healthcare providers. In terms of practice, this review highlighted the clear need for family-centred interventions that focus on providing health education to parents of children with health conditions, as well as enhancing health education in school settings. Furthermore, young people expressed insightful suggestions to improve care, showcasing the need for healthcare providers to elicit young people’s voices and recognize the impact that clinicians may unconsciously have on children’s health experiences. Future researchers may consider conducting a more focused review of the literature pertaining to specific ethical concerns or consequences impacting children. In all, this review provides a foundational body of evidence to serve as a starting point for continued research in the area of children’s perspectives towards their health in India.
Conclusions
The themes identified from this review demonstrated that ill and symptomatic children in India often expressed similar health-related experiences, views, and needs across several domains of life despite their various health statuses, experiences, and backgrounds. These domains were not restricted to their immediate medical milieu, but rather extended to children’s relationships, schooling, and activities of daily living. This scoping review identified key areas for improvement in children’s healthcare including the need to elicit children’s voices during care, provision of adequate psychosocial support, enhancing health education, and training healthcare providers to recognize the impact of their behaviours on children’s health experiences while taking actions to provide appropriate, sensitive care. Given the widespread impacts of health services on other areas of children’s lives, research in healthcare and childhood ethics play an integral part in insuring that these impacts are known and considered by those who make healthcare decisions in children’s best interests. By highlighting this link, our scoping review contributes to children’s healthcare and childhood ethics research. Although more research is needed to fully understand children’s health-related experiences in India, the development of an ongoing dialogue between researchers, healthcare providers, as well as children and families can promote the inclusion of children in their own care and lead to improved health research and practices that are suitable for young people in India.
Acknowledgments
The authors would like to thank Crystal Noronha, Kiesha Dhaliwal, Sarah Khan, Jacqueline Mancini, and the Views On Interdisciplinary Childhood Ethics (VOICE) team for their support, guidance, and contributions in conducting this review. We are also grateful to Angella Lambrou for lending her expertise in designing and conducting the search.
Funding
The following financial supports were received by the authors for the research, authorship, and publication of this article: Justine Behan was supported by the Mr. and Mrs. John Henry Collins Memorial Bursary (grant ID: 260574445); Dr. Argerie Tsimicalis was supported by the Fonds de Recherche Québec-Santé (Quebec Medical Research Council) under the Chercheur-Boursier Junior 1 Award.
Conflict of interest disclosure
The authors report no conflicts of interest.
References
- Carnevale FA, Campbell A, Collin‐Vézina D, Macdonald ME. Interdisciplinary Studies of Childhood Ethics: Developing a New Field of Inquiry. Children & Society. 2015;29(6):511–23. https://doi.org/10.1111/chso.12063
- Söderbäck M, Coyne I, Harder M. The importance of including both a child perspective and the child’s perspective within health care settings to provide truly child-centred care. J Child Health Care. 2011 Jun 1;15(2):99–106. https://doi.org/10.1177/1367493510397624
- WHO. Constitution of the world health organization. Am J Public Health Nations Health. 1946;36(11):1315–23. Available from: https://ajph.aphapublications.org/doi/10.2105/AJPH.36.11.1315
- Kreitzer MJ, Weil A, Koithan M. Integrative Nursing. Oxford University Press; 2018. 745 p.
- Hunt MR, Carnevale FA. Moral experience: a framework for bioethics research. Journal of Medical Ethics. 2011 Nov 1;37(11):658–62. http://dx.doi.org/10.1136/jme.2010.039008
- Gottlieb LN. Strengths-based nursing. Am J Nurs. 2014 Aug;114(8):24–32; quiz 33,46.
- Wang YW, Carnevale FA, Ezcurra M, Chougui K, Bilodeau C, Siedlikowski S, Tsimicalis A. The moral experiences of children with osteogenesis imperfecta. Nursing Ethics. 2022 Dec;29(7-8):1773-91.
- Donnelly M, Kilkelly U. Participation in Healthcare: the Views and Experiences of Children and Young People. The International Journal of Children’s Rights. 2011 Jan 1;19(1):107–25. https://doi.org/10.1163/157181810X522379
- Coyne I, Amory A, Kiernan G, Gibson F. Children’s participation in shared decision-making: Children, adolescents, parents and healthcare professionals’ perspectives and experiences. European Journal of Oncology Nursing. 2014 Jun 1;18(3):273–80. https://doi.org/10.1016/j.ejon.2014.01.006
- Bravo L, Killela MK, Reyes BL, Santos KMB, Torres V, Huang C-C, et al. Self-Management, Self-Efficacy, and Health-Related Quality of Life in Children With Chronic Illness and Medical Complexity. Journal of Pediatric Health Care. 2020 Jul 1;34(4):304–14. https://doi.org/10.1016/j.pedhc.2019.11.009
- Tiwari BN, Bhaskar S, Shanker R, Kale S, Kumar SP, Kumar R. Children in India 2018-A statistical appraisal. Ministry of Statistics and Programme Implementation Government of India Retrieved December. 2018;22:2020. https://www.im4change.org/docs/189Children_in_India_2018_A_Statistical_Appraisal.pdf
- Pappachan B, Choonara I. Inequalities in child health in India. BMJ Paediatrics Open. 2017 Aug 1;1(1):e000054. https://doi.org/10.1136/bmjpo-2017-000054
- Usmani G, Ahmad N. Health Status of Children in India. J Perioper Crit Intensive Care Nurs [Internet]. 2017 [cited 2020 Jul 1];03(01). https://doi.org/10.4172/2471-9870.1000138
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005 Feb;8(1):19–32. https://doi.org/10.1080/1364557032000119616
- Whittemore R, Chao A, Jang M, Minges KE, Park C. Methods for knowledge synthesis: An overview. Heart & Lung. 2014 Sep 1;43(5):453–61. https://doi.org/10.1016/j.hrtlng.2014.05.014
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine. 2018 Sep 4;169(7):467–73.
- Malhotra A, Malhotra R. Some Perspectives on Indian Family Law India. Int’l Surv Fam L. 2001;2001:115–46. Available from: https://heinonline.org/HOL/LandingPage?handle=hein.journals/intsfal8&div=15&id=&page=
- Peters M, Godfrey C, McInerney P, Soares CB, Khalil H, Parker D. Methodology for JBI scoping reviews. The Joanna Briggs Institute Reviewers manual 2015. 2015;3–24.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010 Sep 20;5:69. https://doi.org/10.1186/1748-5908-5-69
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008 Dec;8(1):45. https://doi.org/10.1186/1471-2288-8-45
- Sandelowski M. Qualitative analysis: What it is and how to begin. Research in nursing & health. 1995;18(4):371–5. https://doi-org.myaccess.library.utoronto.ca/10.1002/nur.4770180411
- Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice. Lippincott Williams & Wilkins; 2008. 827
- Das A, Detels R, Javanbakht M, Panda S. Living with HIV in West Bengal, India: perceptions of infected children and their caregivers. AIDS Care. 2017 Jun 3;29(6):800–6. https://doi.org/10.1080/09540121.2016.1227059
- Khan F., Arora S., Chakravarty S., George S. A qualitative study to explore the experiences of adolescents living with cancer. International Journal of Nursing Education. 2012;4(2):202–5.
- Karande S, Kelkar A, Kulkarni M. Recollections of Indian children after discharge from an intensive care unit. Pediatric Critical Care Medicine. 2005;6(3):303–7. https://doi.org/10.1097/01.PCC.0000160659.40315.B3
- Dudeja P, Sindhu A, Shankar P, Gadekar T. A cross-sectional study to assess awareness about menstruation in adolescent girls of an urban slum in western Maharashtra. International Journal of Adolescent Medicine and Health; Berlin [Internet]. 2018 [cited 2020 Feb 4];30(4). Available from: http://search.proquest.com/docview/2309824195/abstract/14077BDB755340ADPQ/1
- Rajagopal S, Mathur K. “Breaking the silence around menstruation”: experiences of adolescent girls in an urban setting in India. (Special Issue: Water, sanitation and hygiene.). Sweetman C, Medland L, editors. Gender and Development. 2017;25(2):303–17. https://doi.org/10.1080/13552074.2017.1335451
- Rani A, Sharma MK, Singh A. Practices and perceptions of adolescent girls regarding the impact of dysmenorrhea on their routine life: a comparative study in the urban, rural, and slum areas of Chandigarh. Journal of Adolescent Medicine and Health. 2016;28(1):3–9. http://dx.doi.org/10.1515/ijamh-2014-0063
- Vashisht A, Pathak R, Agarwalla R, Patavegar BN, Panda M. School absenteeism during menstruation amongst adolescent girls in Delhi, India. Journal of Family and Community Medicine. 2018;25(3):163–8. DOI: 10.4103/jfcm.JFCM_161_17
- Narayanan A, Kumar S, Ramani KK. Spectacle Compliance among Adolescents: A Qualitative Study from Southern India. Optometry & Vision Science. 2017 May;94(5):582–7. https://doi.org/10.1097/OPX.0000000000001070
- Dhawan A, Pattanayak RD, Chopra A, Tikoo VK, Kumar R. Injection drug use among children and adolescents in India: ringing the alarm bells. Journal of Psychiatry. 2016;58(4):387–93. https://dx.doi.org/10.4103%2F0019-5545.196701
- Gupta K, Patel AK, Tiwari SK. A Comparative Study of Beliefs and Attitude Towards Menstruation among Urban and Rural Postmenarcheal Adolescent Girls of Delhi NCR. Journal of Psychosocial Research; New Delhi. 2019 Jun;14(1):31–40. http://dx.doi.org/10.32381/JPR.2019.14.01.4
- Prem Kumar SG, Anil Kumar G, Ramgopal SP, Venkata Srinivas V, Dandona R. A comparative assessment of generalized anxiety, conduct and peer relationship problems among AIDS and other orphaned children in India. BMC Psychiatry. 2016 Sep 21;16(1):330. https://doi.org/10.1186/s12888-016-1042-z
- Mehta K, Ekstrand ML, Heylen E, Sanjeeva GN, Shet A. Adherence to Antiretroviral Therapy Among Children Living with HIV in South India. AIDS Behav. 2016 May 1;20(5):1076–83. https://doi.org/10.1007/s10461-015-1207-7
- Govindharaj P, Darlong J, John AS, Mani S. Children and adolescents’ attitude towards having leprosy in a high endemic district of India. Lepr Rev. 2016;87(1):42–52. https://leprosyreview.org/admin/public/article_shell/uploads/article_files/Lepra/LEPROSY/87/1/lr042052/lr042052.pdf
- Verma M, Verma SP. Coping Strategies and Quality of Life of Adolescents with Asthma. Social Science International. 2013;29(1). https://www.proquest.com/openview/245a84305bcf97ea21f954e0c7312078/1?pq-origsite=gscholar&cbl=506333
- Roy T, Chatterjee SC. The experiences of adolescents with thalassemia in West Bengal, India. Qualitative Health Research. 2007;17(1):85–93. https://doi.org/10.1177/1049732306296400
- Patel AB, Pathan HG. Quality of life in children with sickle cell hemoglobinopathy. The Indian Journal of Pediatrics. 2005;72(7):567–71. https://doi.org/10.1007/BF02724180
- Sanjeeva GN, Pavithra HB, Chaitanya S, Sunil Kumar DR, Rewari BB. Parental concerns on disclosure of HIV status to children living with HIV: children’s perspective. AIDS Care. 2016 Nov;28(11):1416–22. https://doi.org/10.1080/09540121.2016.1189503
- Seenivasan P, Priya KC, Rajeswari C, Akshaya CC, Sabharritha G, Sowmya KR, et al. Knowledge, attitude and practices related to menstruation among adolescent girls in Chennai. Journal of Clinical and Scientific Research. 2016;5(3):164–70. http://dx.doi.org/10.15380/2277-5706.JCSR.15.031.
- Gupte HA, D’Costa M, Chaudhuri L. Why do Adolescents Initiate and Continue Using Tobacco and Areca Nut?: A Qualitative Study Tracing Pathways of Use Among School-Going Adolescents in Mumbai, India. Nicotine & Tobacco Research. 2020 Jan 22. https://doi.org/10.1093/ntr/ntaa015
- Sharma S, Seth B, Jawade P, Ingale M, Setia MS. Quality of Life in Children with Thalassemia and their Caregivers in India. Indian J Pediatr. 2017 Mar 1;84(3):188–94. https://doi.org/10.1007/s12098-016-2267-z
- Verma A, Goswami M, Dhillon JK. Tobacco use among school going children. Indian Journal of Dental Research. 2019 Dec 11;30(6):839–43. https://doi.org/10.4103/ijdr.IJDR_27_18
- Grover C, Goel N, Chugh K, Gaur SN, Armour C, Asperen PP van, et al. Medication use in Indian children with asthma: The user’s perspective. Respirology. 2013;18(5):807–13. https://doi.org/10.1111/resp.12081
- Chauhan GD, Kodnani AH. A study of prevalence and impact of dysmenorrhea and its associated symptoms among adolescent girls residing in slum areas of Vadodara city, Gujarat. Journal of Medical Science and Public Health. 2016;5(3):510–5. https://doi.org/10.5455/ijmsph.2016.20102015145
- Mathiyalagen P, Peramasamy B, Vasudevan K, Basu M, Cherian J, Sundar B. A descriptive cross-sectional study on menstrual hygiene and perceived reproductive morbidity among adolescent girls in a union territory, India. Journal of Family Medicine and Primary Care. 2017;6(2):360–5. https://doi.org/10.4103/2249-4863.220031
- Deepa Lakshmi Kp, Aswath Narayanan M, Ramesh Kumar S, Selvamary Al, Sujatha A. Permanent anterior teeth fractures and its impact on oral health-related quality of life among 8–15-year-old schoolchildren of Chennai City – A cross-sectional survey. Int J App Basic Med Res. 2020;10(1):30. https://doi.org/10.4103/ijabmr.IJABMR_346_18
- Singh A, Dhawan P, Gaurav V, Rastogi P, Singh S. Assessment of oral health-related quality of life in 9-15 year old children with visual impairment in Uttarakhand, India. Dental Research Journal. 2017 Feb 1;14(1):43–9. https://doi.org/10.4103/1735-3327.201132
- Gothwal VK, Sharma S, Mandal AK. Beyond Intraocular Pressure: Visual Functioning and Quality of Life in Primary Congenital Glaucoma and Secondary Childhood Glaucoma. American Journal of Ophthalmology. 2020 Jan;209:62–70. https://doi.org/10.1016/j.ajo.2019.09.002
- Kumar G, Chhabra A, Dewan V, Yadav TP. Idiopathic musculoskeletal pain in Indian children–Prevalence and impact on daily routine. Revista Brasileira de Reumatologia (English Edition). 2017 Jan;57(1):8–14. https://doi.org/10.1016/j.rbre.2015.07.015
- Batra A, Kumari M, Paul R, Patekar M, Dhawan D, Bakhshi S. Quality of Life Assessment in Retinoblastoma: A Cross-Sectional Study of 122 Survivors from India. Pediatric blood & cancer. 2016;63(2):313–7. https://doi.org/10.1002/pbc.25781
- Jodalli PS, Ankola AV, Hebbal M, Vikneshan M. Aesthetic perceptions regarding fluorosis by children from an area of endemic fluorosis in India. Community Dent Health. 2013;30(4):249–53. https://doi.org/10.1922/CDH_3165Jodalli05
- John AS, Rao PS, Kundu R, Raju MS. Leprosy among adolescents in Kolkata, India. Indian journal of leprosy. 2005;77(3):247–53. Available from: https://europepmc.org/article/med/16353523
- Singh V, Ghai A. Notions of self: Lived realities of children with disabilities. Disability & Society. 2009;24(2):129–45. https://doi.org/10.1080/09687590802652363.
- Morjaria P, Evans J, Gilbert C. Predictors of Spectacle Wear and Reasons for Nonwear in Students Randomized to Ready-made or Custom-made Spectacles: Results of Secondary Objectives From a Randomized Noninferiority Trial. JAMA Ophthalmol. 2019 Apr 1;137(4):408. https://doi.org/10.1001/jamaophthalmol.2018.6906
- Tiwari AN, Bansal M, Manju V, Joshi P, Sinha A, Hari P, et al. A Comparative Study to Find out the Health Related Quality of Life of Children with End Stage Renal Disease on Various Renal Replacement therapies: Self and Parental Perception. Inter Jour of Nurs Educ. 2015;7(2):142. https://doi.org10.5958/0974-9357.2015.00092.6
- Gulati S, Paterson M, Medves J, Luce-Kapler R. Adolescent group empowerment: group-centred occupations to empower adolescents with disabilities in the urban slums of North India. Occupational therapy international. 2011;18(2):67–84. https://doi.org/10.1002/oti.294
- Laungani PD. Understanding Cross-Cultural Psychology: Eastern and Western Perspectives. SAGE; 2006. 282 p.
- Noreña Peña AL, Cibanal Juan L. The experience of hospitalized children regarding their interactions with nursing professionals. Revista Latino-Americana de Enfermagem. 2011 Dec;19(6):1429–36. https://doi.org/10.1590/S0104-11692011000600021
- Ullán AM, Belver MH, Fernández E, Serrano I, Delgado J, Herrero C. Hospital Designs for Patients of Different Ages: Preferences of Hospitalized Adolescents, Nonhospitalized Adolescents, Parents, and Clinical Staff. Environment and Behavior. 2012 Sep 1;44(5):668–94. https://doi.org/10.1177/0013916511403802
- Olsen IØ, Jensen S, Larsen L, Sørensen EE. Adolescents’ Lived Experiences While Hospitalized After Surgery for Ulcerative Colitis. Gastroenterol Nurs. 2016 Jul;39(4):287–96. https://doi.org/10.1097/SGA.0000000000000154
- Ahmadi Doulabi M, Sajedi F, Vamegi R, MazaheriI MA, Akbarzadeh Baghban A. Socioeconomic Status Index to Interpret Inequalities in Child Development. Iran J Child Neurol. 2017;11(2):13–25. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5493825/pdf/ijcn-11-013.pdf
- Allin S, Stabile M. Socioeconomic status and child health: what is the role of health care, health conditions, injuries and maternal health? Health Economics, Policy and Law. 2012 Apr;7(2):227–42. https://doi.org/10.1017/S174413311100034X
- Bradley RH, Corwyn RF. Socioeconomic Status and Child Development. Annual Review of Psychology. 2002;53(1):371–99. https://doi.org/10.1146/annurev.psych.53.100901.135233
- Johnston-Robledo I, Chrisler JC. The Menstrual Mark: Menstruation as Social Stigma. Sex Roles. 2013 Jan 1;68(1):9–18. https://doi.org/10.1007/s11199-011-0052-z
- Orringer K, Gahagan S. Adolescent Girls Define Menstruation: A Multiethnic Exploratory Study. Health Care for Women International. 2010 Aug 4;31(9):831–47. https://doi.org/10.1080/07399331003653782
- Riley AH, Slifer L, Hughes J, Ramaiya A. Results from a literature review of menstruation-related restrictions in the United States and Canada. Sexual & Reproductive Healthcare. 2020 Oct 1;25:100537. https://doi.org/10.1016/j.srhc.2020.100537
- Farrand P, Rowe RM, Johnston A, Murdoch H. Prevalence, age of onset and demographic relationships of different areca nut habits amongst children in Tower Hamlets, London. British Dental Journal. 2001 Feb;190(3):150–4. https://doi.org/10.1038/sj.bdj.4800909
- Livesley J, Long T. Children’s experiences as hospital in-patients: Voice, competence and work. Messages for nursing from a critical ethnographic study. International Journal of Nursing Studies. 2013 Oct 1;50(10):1292–303. https://doi.org/10.1016/j.ijnurstu.2012.12.005
- Altundag S, Bayat M. Peer Interaction and Group Education for Adaptation to Disease in Adolescents with Type 1 Diabetes Mellitus. Pak J Med Sci. 2016;32(4):1010–4. https://doi.org/10.12669/pjms.324.9809
- Tenenbaum HR, Winstone NE, Leman PJ, Avery RE. How effective is peer interaction in facilitating learning? A meta-analysis. Journal of Educational Psychology. 2019. https://doi.org/10.1037/edu0000436
- Qualter P, Vanhalst J, Harris R, Van Roekel E, Lodder G, Bangee M, et al. Loneliness Across the Life Span. Perspect Psychol Sci. 2015 Mar 1;10(2):250–64. https://doi.org/10.1177/1745691615568999
- Hislop J, Mason H, Parr JR, Vale L, Colver A. Views of Young People With Chronic Conditions on Transition From Pediatric to Adult Health Services. Journal of Adolescent Health. 2016 Sep;59(3):345–53. https://doi.org/10.1016/j.jadohealth.2016.04.004
- Laverack G. Improving Health Outcomes through Community Empowerment: A Review of the Literature. Journal of Health, Population and Nutrition. 2006;24(1):113–20. Available from: http://www.jstor.org/stable/23499274
- Demetriou C, Ozer BU, Essau CA. Self-Report Questionnaires. In: The Encyclopedia of Clinical Psychology. American Cancer Society. 2015. https://doi.org/10.1002/9781118625392.wbecp507
| Table 2: Summary of main themes and subthemes | ||||
| Major Themes | Sub-themes | |||
| Children recalled detailed health-related experiences in healthcare facilities and communities | Children had vivid memories of favourable and unfavourable events in the healthcare setting and community | |||
| Children expressed both positive and negative emotions related to their health |
Negative emotions primarily arose when children experienced uncomfortable symptoms, uncertainty, and health-related limitations Positive emotions primarily arose when children were knowledgeable about their health, felt supported, and/or maintained a positive outlook |
|||
| Children had varying levels of knowledge regarding their health, treatment, and the consequences of illness |
Children’s health-related knowledge and attitudes were influenced by their sociocultural backgrounds Family and peers were the most commonly reported sources of health-related information which influenced the accuracy and scope of children’s health-related knowledge Most children had incomplete knowledge regarding their illness/symptoms, contributing to distress, confusion, and poor treatment compliance |
|||
| The impacts of health and illness extended beyond children’s physical well-being |
Illness significantly disrupted children’s schooling, social relationships, and day-to-day activities such that children reported unwanted school absences, exclusion from peers and family, difficulties with activities of daily living, and other social and physical limitations and restrictions Illness impacted children differently depending on gender, age, and background |
|||
| Children had the capacity to identify and communicate their health-related needs to clinicians and researchers |
Children understood the additional stressors associated with illness, expressed their need for more psychosocial support, and took into consideration the needs of other ill children when making suggestions to improve care Children spoke openly about their health-related needs and desires when their voices were elicited Children were most empowered in collaborative group settings with healthy peers and youth who have similar conditions |
|||

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.